Birth control pills: Effectiveness, side effects, and alternatives
Key takeaways:
- Birth control pills contain hormones that change how your body works to prevent pregnancy
- There are two main types of birth control pills: the combined pill and the progestin-only pill
- Some people may experience side effects from using hormonal birth control such as the pill, but serious risks to health are rare
What is the birth control pill?
The birth control pill (often referred to as ‘the pill’) is a small, ingestible tablet that contains a combination of hormones. These hormones change the way the female body functions to prevent pregnancy.
What are the types of birth control pills?
There are a few different types of birth control pills available these are:
- The combined pill: This contains a combination of synthetic hormones estrogen and progesterone (progestin) — this is the most common type of prescribed pill.
- The progestin-only pill (POP): Sometimes called the mini pill, this type of contraception only contains the synthetic hormone progesterone. It’s sometimes prescribed for those who can’t take synthetic estrogen (for example, if you are at a higher risk of blood clots),
- The morning-after pill: This is a type of emergency birth control you take once after unprotected sex. There are two common brands of morning-after pills in the US (Plan B and Ella).
Within the two categories of daily birth control pills, there are many different brands available such as Levora, Yaz, and Cerazette. These contain varying levels of hormones, taking your preference and personal medical history into account, your doctor or gynecologist will be able to recommend the right option for you.
How do birth control pills prevent pregnancy?
This depends on the type of pill you’re using. Estrogen in the combined pill works to inhibit ovulation (stops an egg cell from being released). Progestin thickens cervical mucus, making it harder for sperm to survive, in some cases, it can also stop ovulation, but some people using the mini pill will still ovulate.
How effective is the pill?
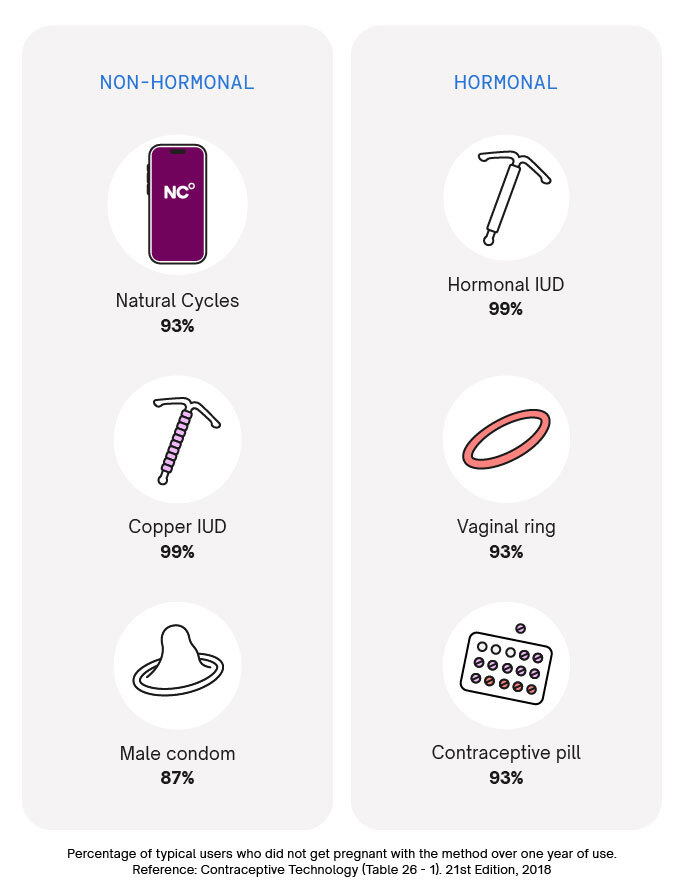
Both the mini pill and the combined pill are more than 99% effective when used perfectly. However, with typical use, they are 93% effective at preventing pregnancy. Typical use reflects how birth control methods are actually used and includes things like forgetting to take a pill or taking a pill late. This means, on average, 7 out of 100 women using the birth control pill will get pregnant over the course of a year.
How long does the pill take to work?
This depends. If you’re on your period, you can start taking the pill and be protected from pregnancy straight away (as you’re unlikely to be fertile at the start of your cycle). If you start taking the combined pill any later than the fifth day of your cycle, you will need to take it for seven days before you’re protected against pregnancy. During this time, you should abstain from sex or use another method of contraception, such as condoms.
If you’re starting the progestin-only pill, you need to take the pill for two consecutive days before you’re protected.
How to take birth control pills
If you’re using the combined pill, you will take a pill every day for three weeks. You will then either have a week’s break in between pill packets, or you’ll take a week’s worth of sugar pills before starting a new packet. During this week, you will experience what’s called a withdrawal bleed (light bleeding that’s a bit different from a regular period).
It’s becoming increasingly common for those who use the combined pill not to take this break and instead run pill packets together. There is no medical benefit to taking a break in pill packets – it all comes down to personal preference. Still, if you take the birth control pill continuously, you may experience breakthrough bleeding.
If you’re using the progestin-only pill, you will take the pill at the same time every day without a break in pill packets. It’s normal for those on this form of birth control to experience light or irregular bleeding. Some people will not have any bleeding at all.
No matter what type of pill you’re taking, it’s important to get into a routine. You may find it helpful to take your pill first thing in the morning or when you brush your teeth at night before you go to bed. It doesn’t matter what time of day you take it, but it’s important you are able to be consistent with when you take it each day.
What should I do if I miss a pill?
If you’re taking the combined pill and you’ve only missed one pill, you’re still protected against pregnancy. Take the missed pill as soon as you realize (even if that means taking two pills on the same day). Continue taking the pill as normal, there is no need to use emergency contraception.
If you’ve missed multiple birth control pills, you may need to use a backup form of birth control for seven days until you are protected again. If you forget to take the sugar pills in week four, that’s OK, you’re protected against pregnancy during this time anyway.
For the progestin-only option, you may not be protected if you’re as little as three hours late in taking this pill. You may need to use a backup method of birth control for two days until you are protected again.
Guidance varies between pill types and brands. Make sure you check with your specific pill’s packet for instructions or ask your OBGYN if you have questions.
What if I vomit or have diarrhea after taking the pill?
If you throw up within three hours of taking the pill, your body may not have properly absorbed the hormones. Treat it as if you’ve missed a pill, and take the next pill in your packet. If you continue to be sick or have diarrhea for a prolonged period of time, you may not be protected against pregnancy and should use another birth control method in the meantime.
If you’ve had sex and are worried about becoming pregnant, you can use emergency birth control up to five days after unprotected sex.
Pros & Cons of taking the pill
As with all birth control methods, there are good and bad things about using the pill as your chosen contraceptive method. It’s important to weigh these up when considering switching methods.
Advantages of the pill:
- It’s effective: When used perfectly, the pill is more than 99% effective at preventing pregnancy, with typical use, it’s still 93% effective.
- It doesn’t take much work: If you’ve got a steady routine, you may find it easy to make taking a pill a daily habit.
- It is non-invasive: Unlike some other popular birth control methods (e.g., IUDs) the pill doesn’t stay in your body — if you choose to stop using it, you can do so quickly without a medical procedure.
- It’s low risk: The pill has been around for a long time and has undergone a lot of testing, while there are some risks attached to using the pill, the serious ones are extremely rare.
- It has other benefits: The combined pill can be used to treat acne, or regulate menstrual cycles if you suffer from heavy bleeding from conditions such as endometriosis.
Disadvantages of the pill:
- You have to remember to take it every day: If your routine frequently changes or you think you’ll struggle to remember to take the pill, it may not be the best option for you.
- There are known side effects: Some people may have unpleasant side effects due to the hormones in the pill. The mini pill and combined pill contain different hormones, so some people may get side effects from one but not the other.
- The pill alters your natural cycle: In order to prevent pregnancy, the pill inhibits ovulation and thickens cervical mucus, while many people don’t mind their body changing in this way, you may prefer to keep their body’s natural rhythm.
- It doesn’t protect against STIs: Since the pill isn’t a barrier method, it doesn’t offer any protection against sexually transmitted infections.
- There is still a risk of pregnancy: No birth control method is 100% effective, and the pill is no exception. If you want to reduce the risk of pregnancy further, you could opt for a highly effective method like an IUD, or use condoms with the pill for extra protection.
- There’s a small chance of more serious risks: Birth control pills have been linked to an increased risk of some health conditions, such as blood clots and breast cancer.
What medications should I avoid while taking the pill?
It’s best to check in with your doctor if you’re taking any medications to check that they don’t interfere with your contraception. Medications that can affect the combined birth control pill include:
- Certain antibiotics (such as rifampicin)
- Some epilepsy drugs
- Some drugs used to treat HIV
- Some antimalarial drugs
- St John’s wort (a herbal remedy)
Are there any side effects to taking the pill?
Yes, there are a number of side effects you may experience on the combined or mini pill. For many people, these will go away within two or three months as your body adjusts, others may find these don’t go away and choose to switch birth control methods. Side effects include:
- Irregular bleeding
- Nausea
- Headaches
- Sore breasts
As outlined earlier, there are also some rarer risks to be aware of when it comes to taking the pill. That’s why you need to consider your own medical history. For example, if you’ve had breast cancer, you should avoid the progestin-only pill. Whereas those with an increased risk of stroke (e.g., those who have migraine with aura) may opt for the mini pill or another birth control method without estrogen. Talk to your doctor to learn more about what’s the best option for you.
Does the pill protect against STIs?
Using the birth control pill will not protect you against any type of sexually transmitted infection. The good news is that you can still use condoms with the pill, not only will they protect you against sexually transmitted infections, but they offer another layer of protection against pregnancy.
What are alternatives to the pill?
Not everyone is able to take the pill or wants to use this method of birth control, so it’s important to be aware of more options out there. We recommend always talking to your doctor before you switch methods, but it’s good to know what’s out there. A few alternatives to the pill include:
- Intrauterine devices (IUDs): More than 99% effective at preventing pregnancy, IUDs come in both hormonal and non-hormonal versions. The device must be fitted and removed by a healthcare professional, but once fitted lasts for a maximum of 12 years.
- Natural Cycles: A hormone-free alternative, Natural Cycles is a temperature-based birth control app, that learns the pattern of your cycle to find fertile days. With typical use Natural Cycles is 93% effective, and 98% effective with perfect use. Natural Cycles is FDA Cleared in the US and CE marked for use as contraception in Europe.
- Birth control shot: This is another option for those who can’t take synthetic estrogen. The shot is given approximately every twelve weeks and is 96% effective with typical use and more than 99% effective with perfect use.
- The ring: The vaginal ring contains similar hormones to the combined pill and is just as effective. The ring is inserted into the vagina and worn for 21 days, followed by a week’s break before the cycle begins again.
- The patch: The birth control patch has similar effectiveness to the pill and the ring, except it’s worn on the skin and changed every week – after three weeks, you take a week’s break.
- Condoms: A great option if you also want to protect against STIs, this hormone-free option must be used every time you have sex (if you’re using them as your only birth control). With typical use, condoms are 87% effective and 98% effective with perfect use.
Thinking about going hormone-free?
Thanks for reading up on the birth control pill — we hope you’ve learned a lot about this popular contraceptive option. If you’re thinking about switching birth control, why not consider a non-hormonal option?
Natural Cycles has helped over 3 million users plan or prevent pregnancy naturally, without any side effects. The NC° algorithm adapts to you — it’s designed to work with your cycle, even irregular ones! Click 'Start my joruney' to take our quiz and find out if NC° could work for you today.
Did you enjoy reading this article?



