Vasectomy procedure: recovery & effectiveness
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Vasectomies are safe, effective, non-hormonal birth control procedures
- They are performed as an outpatient procedure, and recovery time is typically quick with limited discomfort
- Vasectomies do not protect against sexually transmitted infections as barrier methods like condoms do
If you or your partner is curious about a vasectomy as a form of birth control, in this article, you'll learn about what a vasectomy procedure entails, vasectomy recovery information, and some pros and cons of this contraceptive choice.
Vasectomy is one of the most common forms of male birth control in developed nations. It accounts for 10.8% of contraceptive methods as reported by women in the United States, 21.7% in Canada, 21% in the UK, and 16.4% in Western Europe [1]. Let’s dive in and explore why this procedure is being chosen.
What is a vasectomy?
A vasectomy is a simple surgical procedure that is also referred to as “male sterilization.” Vasectomies are generally considered safe with minimal risk for the patient. Most of the time, the procedure is quite quick with patients able to go home the same day [4].
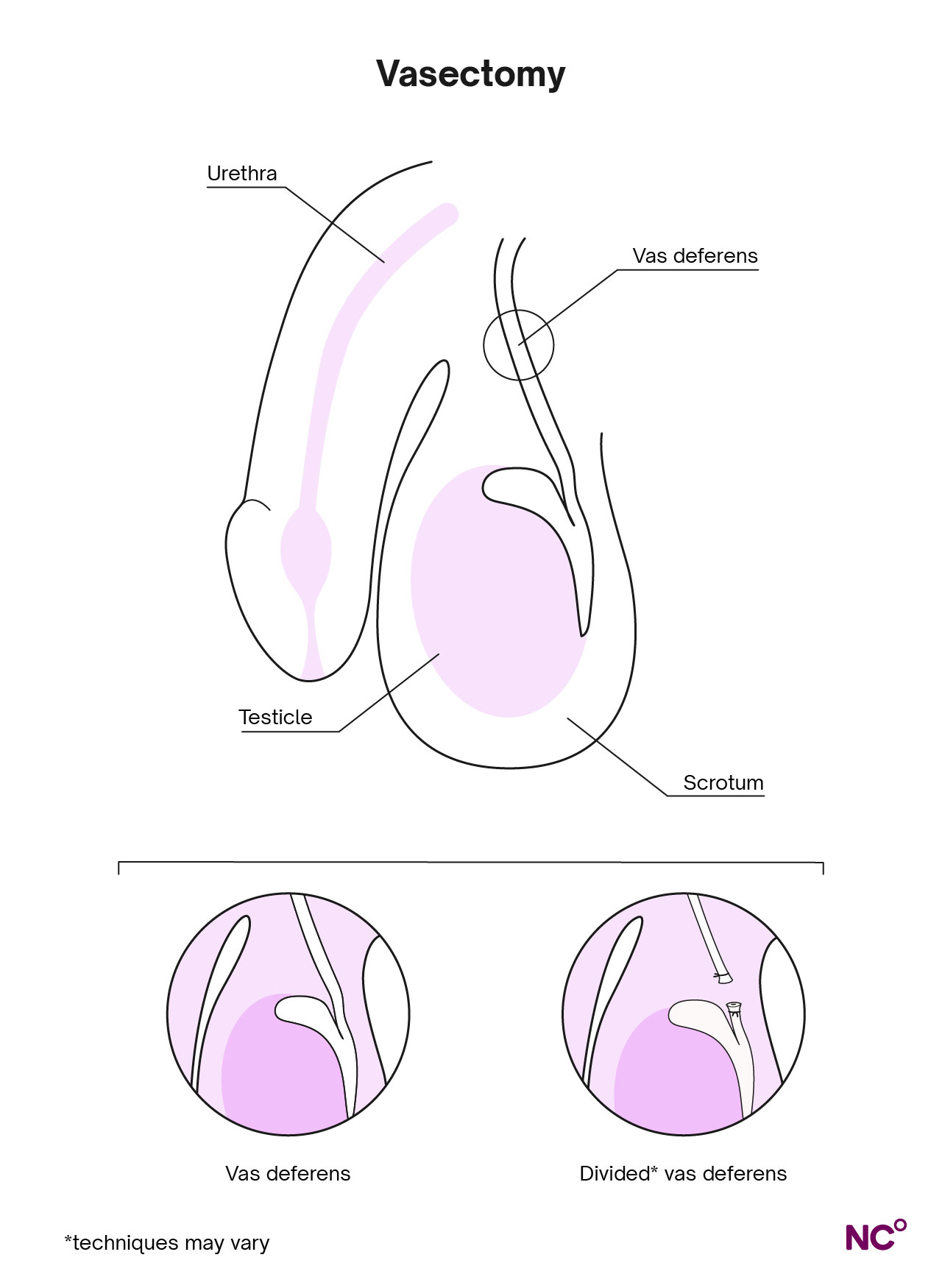
The procedure involves cutting or blocking the vas deferens — the small tubes in the scrotum that carry sperm cells from the testicles to the ejaculatory duct, where it mixes with other liquids to become semen that is ejaculated from the penis [4]. Closing off these tubes prevents sperm from mixing with semen, leaving the body, and fertilizing a female egg cell during sex, thus effectively preventing pregnancy [3].
Patients are still able to ejaculate post-operation, and there will be barely any difference in the semen (sperm only make up about 5% of semen fluid) [3]. The body still produces male sex hormones and sperm as well — the sperm cells will just be safely reabsorbed into the body rather than transferred to the female egg cell [4].
It’s important to note that vasectomies do not prevent sexually transmitted infections or diseases as condoms do, but they are a highly effective birth control method otherwise [3].
How effective is a vasectomy?
Vasectomy procedures are among the most effective methods of birth control to prevent pregnancy [5]. While no form of contraception can guarantee 100% effectiveness, the risk of pregnancy is extremely low with vasectomies. They are more than 99% effective at preventing pregnancy as long as post-operative instructions are followed [5].
Keep in mind that vasectomies are only effective after the sperm count in your partner’s semen is non-moving and near zero [6]. Your doctor will perform follow-up tests in the months following the vasectomy to measure your sperm count, usually about two to four months after the procedure [6]. This buffer period is needed to make sure all existing sperm (created and dispersed before the procedure) has time to clear. As a couple, you’ll need to use another form of birth control to prevent pregnancy until your doctor can confirm your ejaculate is free of sperm [3].
There is no evidence that vasectomies cause erectile dysfunction, reduce orgasms, decrease sexual interest, or diminish pleasure [6]. Instead, studies have actually seen an increase in intercourse frequency or improvement in sexual satisfaction for most men (and female partners) after a vasectomy [2].
Vasectomy procedure explained
Now that we’ve gone over the basics, let’s dive into the details of the vasectomy procedure:
What happens before a vasectomy?
Before the procedure, the doctor will do a consultation going over medical history, logistics, benefits, risks, interactions with any medications the patient is currently taking, along with post-operative care [6].
On the day of the vasectomy, the area will be shaved and washed with an antiseptic. The patient will receive local anesthesia, and possibly general anesthesia or an oral sedative depending on what the doctor prescribes [6]. The anesthesia will numb any sharp pain, but the patient may still feel some sensation like touch, tension, or tugging [4].
How is the vasectomy procedure done?
Vasectomies are out-patient procedures typically done by a surgeon or urologist. There are two main techniques for vasectomies: incision (also called “conventional” vasectomy or CV) and no-cut (also called “no-scalpel” vasectomy, which is an example of “minimally invasive” vasectomy or MIV) [4, 6]. Let’s go through each type, as they’re performed a bit differently:
What happens during an incision vasectomy?
During a conventional or incision vasectomy, one or two small cuts are made to open the skin of the scrotum. From that opening, one of the vas deferens tubes is pulled through until it forms a loop. Then, a small section of the tube is cut out, and the two ends are tied. They may also be sealed with heat, which causes scar tissue to form over time and further block the tubes. This process is repeated for the other tube, and then each is put back in place. The cut skin may be closed with dissolvable stitches or allowed to heal and close on their own depending on the case. [3, 4].
What happens during a no-scalpel vasectomy?
The no-cut or no-scalpel vasectomy technique was developed more recently in the 1970s. This procedure still involves blocking the tubes, but no incisions are made on the skin. Instead, the vas deferens is first located and held into place with a clamp through the skin before a special tool is used to puncture the scrotum in one place. The tubes are then gently pulled up through the small hole, blocked, and put back into place. This means that no stitches are needed, and there tends to be less post-operative pain along with shorter recovery time [3, 4].
Does getting a vasectomy hurt?
It’s normal to experience some mild pain or slight discomfort over the first few hours/days after the procedure, but chronic, ongoing pain is extremely rare, affecting only about one to two percent of patients [6]. Light over-the-counter pain medication should help with the discomfort after the procedure [4].
A benign lump called a granuloma may also appear in the days following the vasectomy. This happens because sperm may leak from the cut end of one of the tubes into the scrotal tissues. It may be a bit painful or sensitive to touch, but it isn't harmful and will likely subside with time [4].
Vasectomy recovery: what you need to know
There are quite a few things to keep in mind post-op which we’ll go over on a high level below. Remember that the doctor will cover specific, personalized vasectomy recovery information related to each case, including guidance on what medications to take, or what to do in the case of certain health conditions.
What happens after you have a vasectomy?
After the vasectomy, post-op care instructions usually include lots of rest following the procedure. Your doctor may also suggest an ice pack for swelling or pain, along with compression underwear or a jockstrap to aid with recovery. Following the instructions as closely as possible is recommended for the quickest, healthiest recovery. [4]
How long does it take to recover after a vasectomy?
While the patient is usually able to go home the same day of the vasectomy procedure, they’ll still need to rest for at least one day. Most people are able to return to their job as early as the next day if they do sedentary desk work, and within the following week otherwise [4].
When is it safe to have sex after a vasectomy?
It’s best to avoid sex or ejaculation for three to seven days during vasectomy recovery. Any other activities that involve a lot of strength or endurance should also be avoided if possible [4].
When can you stop other forms of birth control?
As we mentioned earlier, sperm cells can remain in the vas deferens tubes for weeks or months after the vasectomy, so you and your partner will need to use another form of birth control until your doctor confirms that there are no motile sperm left in the semen [6].
Can I have a vasectomy reversed later if I choose?
While the procedure can be reversed in some cases, it’s never guaranteed and the success rate of reversal is dependent on a number of variables you can discuss with your doctor. Vasectomy reversals may also be expensive and not covered by insurance [7].
With that in mind, make sure you and your partner discuss if you want to have any (or more) children before getting a vasectomy. If you’re not settled on that point but you still want to have the procedure done, you might want to consider freezing a sperm sample before the vasectomy [3]. There are a few procedures, aside from vasectomy reversal, that may still allow you to get pregnant with a sperm sample. These include in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). Again, keep in mind that these procedures can be expensive and the success rate is about one in every two couples who try these techniques [6].
It’s worth noting that across a large number of studies, only about one to two percent of men expressed regret or dissatisfaction about having undergone vasectomies, while the great majority would recommend it to others [6].
Pros and cons of vasectomy procedures
Let’s recap what we’ve learned so far with some pros and cons:
Pros of a Vasectomy:
- You don’t need to think about this birth control method every day or every time you have sex
- Vasectomies are more than 99% effective at preventing pregnancy
- It’s a quick outpatient procedure with minimal downtime
- It’s often more affordable, effective, and safe than the female sterilization alternative, tubal ligation (even so, tubal ligation remains more common than vasectomy in the U.S., even among married couples who are looking for permanent sterilization [6])
Cons of a vasectomy:
- Mild pain and discomfort post-procedure
- Does not protect against sexually transmitted infections
- Invasive birth control method (surgery is required)
- Very slight risk of complications like infection or swelling
When to speak with a doctor
It’s best for you and your partner to speak with your healthcare provider about your specific case if you’re curious about getting a vasectomy to make sure it’s the best option for you. They’ll go over the risks, benefits, and what you can expect from the procedure if you decide to move forward.
Post-operation, contact your doctor as soon as possible if you notice:
- Scrotum is enlarged
- Scrotum is red or sore
- Fever
- Continued pain [4]
Take control of your reproductive journey with Natural Cycles
At Natural Cycles, we’re passionate about birth control choice and want you to have an awareness of all your options, including more permanent methods like sterilization. We also believe that contraception is a shared responsibility among couples. Dr. Brian Nguyen, member of the Natural Cycles Medical Advisory Board, shared his perspective with us.
“While pregnancy prevention is commonly thought of as a woman’s responsibility, prior to the development of female hormonal contraception, men were primarily responsible via their use of condoms and/or withdrawal for contraception. The shift towards female responsibility is thus rather recent, though so widespread that men’s involvement seems so limited today. However, decisions to plan and prevent pregnancy are a couple’s issue that warrants communication between partners about their expectations for family planning,” he said.
If you’re looking for a hormone-free contraceptive method, why not find out if Natural Cycles could work for you? It’s the first FDA Cleared non-hormonal birth control app and uses the science of body temperature to predict ovulation, giving you a deeper understanding of your fertility. No hormones. No Side effects. Just science. Try Natural Cycles today.
Did you enjoy reading this article?
