Tubal ligation: Procedure, recovery & side effects
Follows NC° Editorial Policy
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Tubal ligation is a surgical procedure designed to provide permanent birth control for people who no longer want to get pregnant
- It involves closing off the fallopian tubes so that egg cells cannot be fertilized by sperm cells, thus effectively preventing pregnancy
- Tubal ligation and other sterilization procedures do not protect against sexually transmitted diseases and infections
Tubal ligation is a safe and effective surgical birth control procedure. It’s also commonly referred to as “female sterilization” medically or “getting your tubes tied” conversationally [1]. It’s over 99% effective at preventing pregnancy, making it one of the surest forms of contraception available [2].
Curious about tubal ligation, but still have questions about the procedure? In this article, we’ll answer some FAQs about tubal ligation including what you can expect from the surgery itself, plus information about the tubal ligation recovery process. Use this article as a jumping off point — remember to consult your healthcare team about your goals and medical history before making any major surgical decisions.
What is tubal ligation?
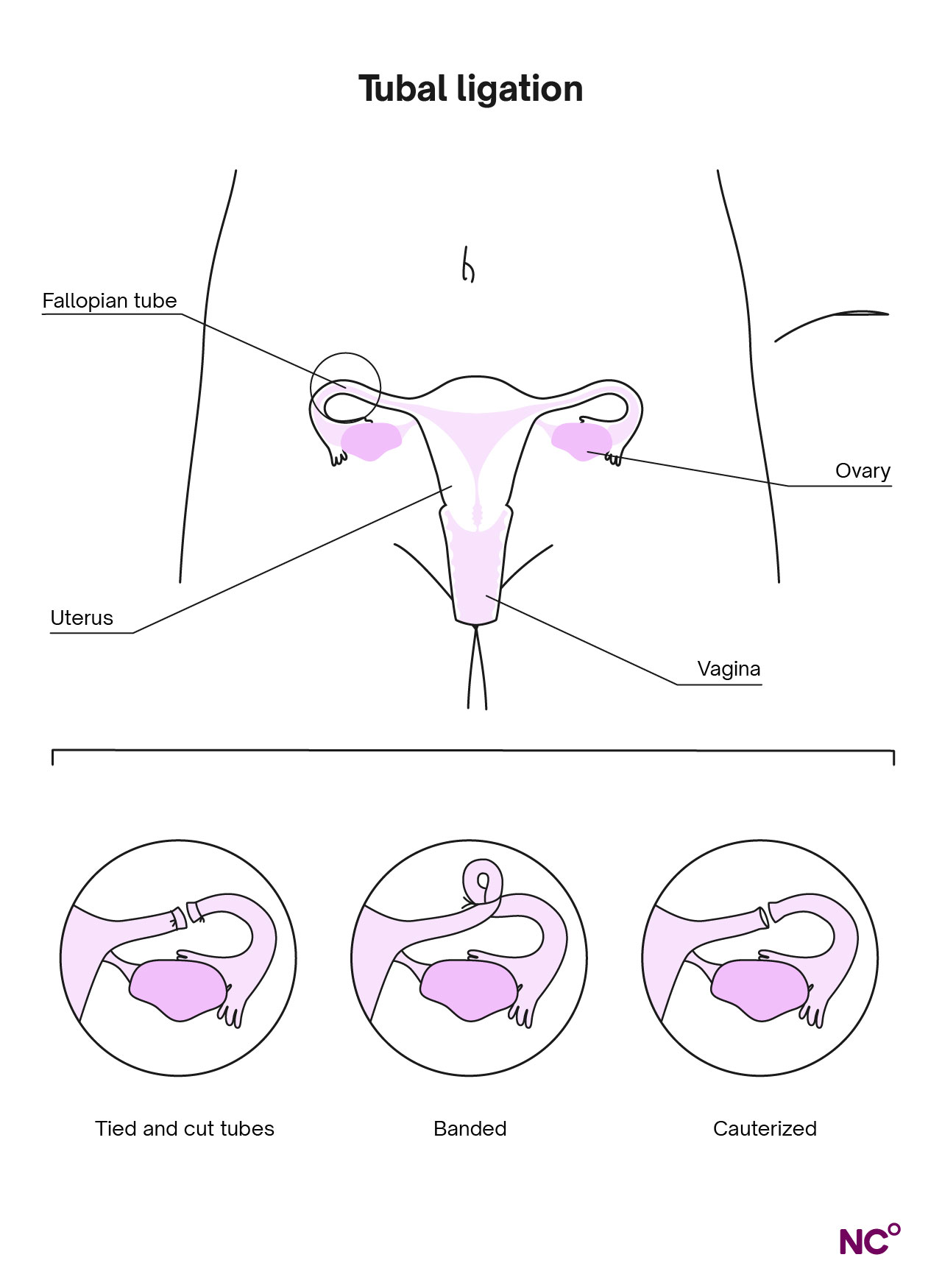
Let’s start with the basics. At a high level, a tubal ligation involves blocking your fallopian tubes, whether that’s by tying them, cutting them, or removing parts of them (more on the different methods used during the procedure later) [1].
The fallopian tubes are located on either side of the uterus and extend toward the ovaries. They receive egg cells from your ovaries once a month and transport them to your uterus. The eggs either get fertilized or they exit the body during your period later in your menstrual cycle [1]. You can get this procedure at any time, including right after childbirth or at any point during your menstrual cycle [3].
With that in mind, if the fallopian tubes are blocked, sperm cells cannot reach or fertilize the egg cells, thus preventing you from becoming pregnant. After tubal ligation, your body will still release an egg cell during ovulation each cycle, but instead of moving through the tubes to your uterus, it will break down and be absorbed by your body just like any other cells your body isn’t using. This means that you’ll still have a monthly period where the uterine lining sheds, just without the egg cell reaching the uterus [1].
Why do people get their tubes tied?
Tubal ligations are typically performed for people who are sure that they don’t want to get pregnant in the future. This may be the case for a variety of reasons — it’s possible that they don’t want to get pregnant at all or that they’ve had all the children they want. It’s a very personal decision based on your lifestyle, genetics, and more [4].
Dr. Karen Tang, member of the Natural Cycles Medical Advisory Board, shared her professional opinion with us. “You should only consider a tubal or vasectomy if you’re 100% certain you do not desire future fertility,” she said. “For women and people with a uterus, sterilization is usually done via salpingectomy now (removal of both fallopian tubes) and this is not reversible, so you’d need IVF to conceive if you changed your mind. If you’re even a little bit unsure, you should choose a method that is not permanent.”
It’s always best to consult with your healthcare provider about the decision to get your tubes tied. Most won’t recommend making this decision during times of high stress and/or if you’re under pressure from a partner or others [5].
Effectiveness rate and failure rate of tubal ligation
Tubal ligation is one of the most effective forms of birth control available. Fewer than one out of every 100 women will get pregnant following the procedure. That effectiveness can be credited to the fact that tubal ligation is permanent and starts working immediately. Also, there’s no way it can be used the wrong way, like other long-acting birth control methods (such as IUDs and implants). It’s a “get it and forget it” type of contraception [1].
Tubal ligation procedure
Still, tubal ligation is a surgical procedure that calls for proper preparation and recovery. Let’s go through some of the most commonly asked questions about tubal ligation to see if it’s a good choice for you to explore with your doctor.
How do I get ready for tubal ligation surgery?
In the days or months prior to the procedure, your healthcare provider will probably have a conversation with you about your reasons for wanting permanent birth control, while discussing other contraceptive options available to you. If you settle on tubal ligation as the path forward, they’ll also go over the risks and benefits of it, the details of the procedure itself, any possible reasons why the surgery may not work, and recovery information (like any other surgery consultation).
They’ll also discuss scheduling — tubal ligation can be done at any time, but if you’re pregnant, keep in mind that you can also get a tubal ligation shortly after giving birth during the same hospital stay. Once these initial preparatory conversations are complete, they’ll ask you to sign consent documents and schedule the surgery [3].
What happens before the procedure?
In the week or so before the tubal ligation procedure, you may need to stop taking any blood clotting medications like aspirin and ibuprofen [4]. You may also be asked to take a pregnancy test (if the surgery isn’t being done post-childbirth) to be sure you aren’t pregnant at the time of the surgery [1].
It’s likely that the doctor will tell you not to drink or eat anything for some time before your surgery, and will give you other detailed instructions on how to prepare including at what time to arrive [4].
How is tubal ligation performed?
There are two main types of tubal ligation procedures: laparoscopic and minilaparotomy. Both methods involve closing off or removing the fallopian tubes so that egg cells cannot be fertilized. Either way, you’ll receive anesthesia so that you won’t be able to feel pain, but the type of tubal ligation you get depends on your circumstances. Let's go through the logistics of each one.
Laparoscopic tubal ligation: This method is typically done with general anesthesia, and if you haven’t just gone through childbirth. Once you’re asleep, the doctor will pump gas into your belly to see the organs, and will make a small incision near the belly button. A device called a laparoscope is then inserted into that small incision. It has a light and lens to allow the surgeon to see the fallopian tubes. Once the tubes are located, the surgeon will use heat, clips, or rings to close them. The device is then removed and you’re all done! The entire procedure takes about 20-30 minutes and there is usually very little scarring [1, 6].
Minilaparotomy tubal ligation: This alternative method is usually done right after childbirth and involves either local or general anesthesia, or an epidural from the delivery. There will still be an incision made near the belly button if you had a vaginal delivery. If you had a cesarean section, the same incision from that surgery will be used for the tubal ligation procedure. The surgeon brings the fallopian tubes up through the incision and either closes them off with a special thread, or removes parts of the tubes. They’re put back in place and the incision is closed with stitches and/or a bandage [1, 7].
Your doctor may also want to discuss a similar surgical procedure called a salpingectomy with you, as Dr. Tang mentioned earlier. This is when the fallopian tubes are removed entirely, and may be recommended if you’re at increased risk for certain cancers [1].
Tubal ligation recovery
What should I expect after getting my tubes tied?
After the procedure, you’ll be taken to a recovery area for monitoring as the anesthesia wears off. If you had a laparoscopic tubal ligation, you’ll probably be allowed to go home within just a few hours (you’ll need a ride home). If you’ve had a minilaparotomy, your doctor may recommend staying overnight for more monitoring. If you had the procedure done after childbirth, you’ll already have a hospital stay scheduled and the tubal ligation shouldn’t add extra time to that stay [1].
How long does it take to recover from a tubal ligation?
This is very dependent on your circumstances, specifically what type of surgery you had and your health. If you had a laparoscopic procedure without childbirth, you should be able to go back to your normal daily activities within a few days (make sure to check in with your body and be sure you’re feeling better before returning to your normal schedule). A minilaparotomy with childbirth will take longer, since it generally takes several weeks to months to recover from childbirth anyway [1].
You’ll be given post-operative instructions from your healthcare provider, and it’s important to follow these closely to ensure a smooth recovery. You’ll likely have at least one follow up appointment with your doctor in a few weeks to make sure you’ve healed from the tubal ligation and remove any stitches if necessary [1].
When is it safe to have sex after getting my tubes tied?
Check with your healthcare provider about when it’s safe to have sex again. As we mentioned earlier, tubal ligation works right away, so you won’t have any risk of getting pregnant, but your body will still be healing for at least a few days and up to a few months if the surgery was done in conjunction with childbirth. It’s best to wait until you’re fully healed to have sex after childbirth or after tubal ligation surgery in general [1].
Do you get your period after you get your tubes tied?
Yes, you’ll still get your period after tubal ligation [5]. Your ovaries will still release eggs, your body will still produce the reproductive hormones it normally does, and your uterine lining will still shed each cycle. The egg cells just won’t be able to reach your uterus anymore.
You may also notice some vaginal discharge or bleeding in the days following the surgery. This is normal, but call your doctor as soon as possible if that’s accompanied by rash, swelling, fever, dizziness, nausea, or any other signs of infection [1].
Can I still get an STD if I have my tubes tied?
Yes, you can. STDs and STIs are typically transmitted via direct contact with skin, semen, or pre-cum, so while sterilization procedures like tubal ligation prevent pregnancy, they do not prevent the spread of STIs. Using external or internal condoms is still the best way to lower your chance of getting or spreading infection, even if you get a tubal ligation.
What are the side effects of having a tubal ligation?
You may have some discomfort and pain around the abdomen after the procedure, and you’ll likely be tired. You may also experience some swelling and changes to your bowel movements. Your healthcare provider will prescribe pain medication if necessary, or let you know which over-the-counter pain medication is best for you. You may also notice shoulder pain — this is from the gas used during the surgery. It can be relieved by lying down [4]. In general, side effects from tubal ligation are usually pretty mild, but remember that resting is important when it comes to recovery from any surgery.
What is post-tubal ligation syndrome?
While it isn’t common, some patients experience some or all of the following abnormal symptoms after the procedure:
- Painful sex
- Low back pain
- Irregular periods (that weren’t irregular before surgery)
- Menopausal symptoms
These postoperative symptoms are referred to as “post-tubal ligation syndrome,” or PTLS. It’s not clear why this happens to some patients, and because research is limited in this area, there isn’t a clear treatment for the syndrome. Your doctor may still be able to treat the symptoms though, so be sure to mention them if you’re struggling [8].
Can I have the procedure reversed later if I choose?
It is sometimes possible to reverse tubal ligation, but sterilization reversals (for both vasectomies and tubal ligations) are often quite costly and complex procedures. Also, there are no guarantees that you’ll be able to get pregnant after the reversal [1]. Dr. Tang shared her perspective with us about tubal ligation reversals.
“Some tubal sterilizations could be reversed (only if most of the tube was left in place, and only a small amount of the tube was cut, clipped, or removed). However, these would be very costly surgeries as they are not covered by insurance, surgeons who can perform tubal reversals especially are rare, and for tubal reversal there’s a risk of ectopic pregnancy (when pregnancy grows outside the uterus) from tubal scarring, or scar tissue could prevent the tube from functioning,” she said.
So overall, while it may be possible, the risks of reversal are fairly high and it’s best to consider tubal ligation a permanent birth control procedure. If you’ve already had tubal ligation but you’re looking for alternative ways to get pregnant, IVF is one option to consider [4]. Anyone considering tubal ligation should consider it a permanent birth control option. If you’re not sure whether or not you’d like to get pregnant in the future, a long-acting birth control option like a copper IUD (that works for up to 10 years) may be a better fit.
Pros and cons of tubal ligation
Although tubal ligation is a very safe and effective birth control method, it isn’t right for everyone. Make the most of your initial consultation with your healthcare provider to be sure you understand all of the pros, cons, and risks associated with the procedure before you make your final decision. Here are some common points to consider:
Pros:
- Effective: It’s a highly effective form of birth control, more than 99% effective at preventing pregnancy [2].
- Convenient: If you’re sure you do not want to get pregnant in the future, you never have to worry about follow up appointments, renewing or replacing birth control, or using it daily or every time you have sex like some other birth control methods.
- Low risk: The procedure has very low chances of complications. Most reported complications are related to anesthesia rather than the procedure itself [7].
- Non-hormonal: Tubal ligation is a non-hormonal birth control that won’t mess with your hormones or your cycle, and it won’t cause any of the hormonal birth control side effects that some people struggle with [1].
Cons:
- Reversal difficulty: As we’ve discussed, the tubal ligation reversal process — when possible — is complex, costly, and may not result in fertility.
- Regret: Some patients ultimately regret getting the procedure — this is most common for women who get their tubes tied before the age of 30 [4].
- Risks: Like with all surgeries, there are risks of bleeding, pain, infection, or poor reactions to the anesthesia. These are rare, but certain conditions like obesity, diabetes, or past abdominal surgeries may increase your risk of complications [3, 8]. It’s also worth noting that in very rare cases, some women have an ectopic pregnancy after getting tubal ligation [7].
- No protection against STDs: You will not be protected against sexually transmitted infections after you get tubal ligation, so you may still need to use condoms if you’re at risk [1].
If you’ve consulted with your doctor and weighed these pros and cons, we hope you’ll have a good idea of whether this birth control method is right for you. If you’re not ready for permanent birth control like this, but you like the idea of a highly effective and convenient birth control, discuss methods like the IUD or the implant with your doctor. Both have over 99% effectiveness and can last for several years [2].
Explore non-hormonal birth control with Natural Cycles
Overall, tubal ligation is a highly effective, convenient, non-hormonal birth control procedure best suited for someone who is sure that they do not want to get pregnant in the future. “Talk with your gynecologist about your particular situation including your preferences, concerns, anatomy and medical history, risk factors, goals for future fertility, to help determine which method would be the best fit for you,” said Dr. Tang.
If you like the idea of non-hormonal contraception, but you’re looking for a non-invasive method, see if Natural Cycles is a good fit for you. It’s the first FDA Cleared non-hormonal birth control app that works with your body to prevent pregnancy.. Explore Natural Cycles contraception today.
Did you enjoy reading this article?



