33 Weeks pregnant: Baby development, symptoms & signs
Key takeaways
- More visits to your healthcare provider during these weeks means more opportunities to ask questions about your health, your baby’s condition, and childbirth
- You can go into labor before your water breaks — remember that contractions, dispelling your mucus plug, and breaking waters are all signs of the latent, or first, stage of labor
- Strengthening your pelvic floor can help with many late pregnancy symptoms and during labor
Welcome to week 33 and your eighth month of pregnancy! With only seven weeks left to go, it is likely you have a lot on your mind right now. Constant appointments, sleepless nights, and various aches and pains can make day-to-day life challenging. Try to prioritize your comfort and health in these final weeks. In this article, we will talk about managing sleeplessness and discuss the early signs of labor. We will also see how your baby is developing, and talk about some new symptoms you might be experiencing this week. Finally, we will offer some tips on things you can do this week to take care of yourself and prepare for meeting your little one.
Your body — and life — at Week 33
Sleepless nights
At 33 weeks, it is possible that you have been dealing with sleep disruption or even insomnia for weeks or months, or this might be something new. As your baby grows, it is increasingly common for physical discomfort to make it difficult to find a comfortable position [1, 2]. Frequently needing to urinate, strange dreams, or stress can also disrupt your sleep. It is recommended to avoid caffeine later in the day, as well as use a pillow (or many pillows) to support your back, belly, and between your knees [1]. It can also be helpful to get some light exercise, if it is considered safe during your pregnancy. This can include prenatal yoga or pilates, water walking or swimming, or taking walks outside.
While sleeping poorly can be a common side effect at the end of pregnancy, prolonged sleep deprivation can have serious effects on your mental health. Sleeplessness and insomnia during pregnancy are also more likely if you are already suffering from depression [3]. If you find that you are feeling increasingly hopeless or if you have lost interest in things you used to previously enjoy, it’s important to contact your healthcare provider [1, 2]. You don’t need to go through this alone and help is available.
So many appointments
During the final months and weeks of your pregnancy, you might find that you have more and more appointments with your OBGYN, nurse, or midwife. This is completely normal. As you get closer to giving birth, it is important to monitor your blood pressure and check your urine frequently as high blood pressure and protein in the urine are the earliest signs of preeclampsia. Preeclampsia is a serious condition that doctors believe to be caused by issues with the placenta [3]. Early detection is important to ensure a healthy delivery for both mother and baby.
Later third trimester appointments are also important for monitoring both the baby’s health and position in the uterus. While these increased appointments might seem tedious, or even stressful, remember that you can use them to ask any questions you might have about birth or labor.
Thinking about labor - early signs
As you get closer to giving birth, it might be time to familiarize yourself with the basics of childbirth. What are the first signs you might be going into labor? What kinds of things can you expect?
Contrary to whatever you might have seen in movies or television shows, labor does not always start with your water breaking - although, of course, it can! It is important to remember that labor can progress at any speed. Understanding the early signs and stages of labor can help you stay calm and know what to do when the time comes.
The first stage of labor is referred to as the latent stage. This is when your cervix starts to dilate, or open, so that your baby can be born. It is usually the longest stage of labor - for some women, it can take hours or even days [4]. Early signs you are going into labor are that you discharge your mucus plug (the jelly-like pink discharge that has been inside your cervix), your water breaks, or you start to feel contractions or tightenings [5]. You might experience just one or all three of these signs.
Labor contractions occur when your womb tightens and then releases, causing discomfort or pain in your pelvic area that can often be felt in your back and abdomen. Unlike Braxton Hicks contractions, labor contractions will come at regular intervals and get stronger as labor progresses. Your first contractions can be mild, or quite painful. Dilation of the cervix (how open your cervix is) and frequency of contractions indicates to your healthcare team how far along your labor is more so than the strength of your contractions [4].
Your water can break before you go into labor, but it can also happen during labor. If your water breaks before you go into labor, you might feel a slow leaking of fluid or experience a sudden uncontrollable gush of water [5]. Amniotic fluid is clear and pale, and it can sometimes be hard to tell the difference between amniotic fluid and urine. Amniotic fluid also might have a little blood in it at the beginning, which can make it slightly pink in color [5]. If you suspect your waters have broken, contact your healthcare provider immediately.
If you have a show (expel your mucus plug) or you begin having contractions, keep monitoring your symptoms. It is recommended that you keep hydrated, rest, and try to stay comfortable [5]. Depending on where you will give birth, different hospitals or birthing centers have different guidelines regarding when you can be admitted. Check with your hospital or birthing center, or speak to your midwife so you know how to proceed when your labor begins. Keeping track of the frequency and duration of your contractions is usually the best way to communicate to your healthcare team the stage of your labor.
In all cases, you should contact your midwife or maternity unit immediately if you experience any of the following [5]:
- Vaginal bleeding
- Your baby is moving less than normal
- You think you are in labor and are less than 37 weeks pregnant
- Your contractions are lasting longer than two minutes
- You are having six or more contractions within a span of 10 minutes
Your baby’s development at 33 weeks
At 33 weeks pregnant, you are in your eighth month of pregnancy. Between weeks 32 and 37, your baby will likely move into a head-down birthing position. The midwife or nurse at your appointments will be regularly checking the baby’s position.
Your baby’s skull is growing, but will remain flexible through the first year to year and a half of life. The bones in your baby’s skull are not connected, or fused, which enables them to fit through the birth canal without causing any damage to the brain [6]. Because of the tight journey during birth, it is also not uncommon for your baby to be born with a slightly misshapen or even pointy head! This is completely normal. During your baby’s first year, the brain grows very quickly, which is why some sutures of the cranium remain flexible [6].
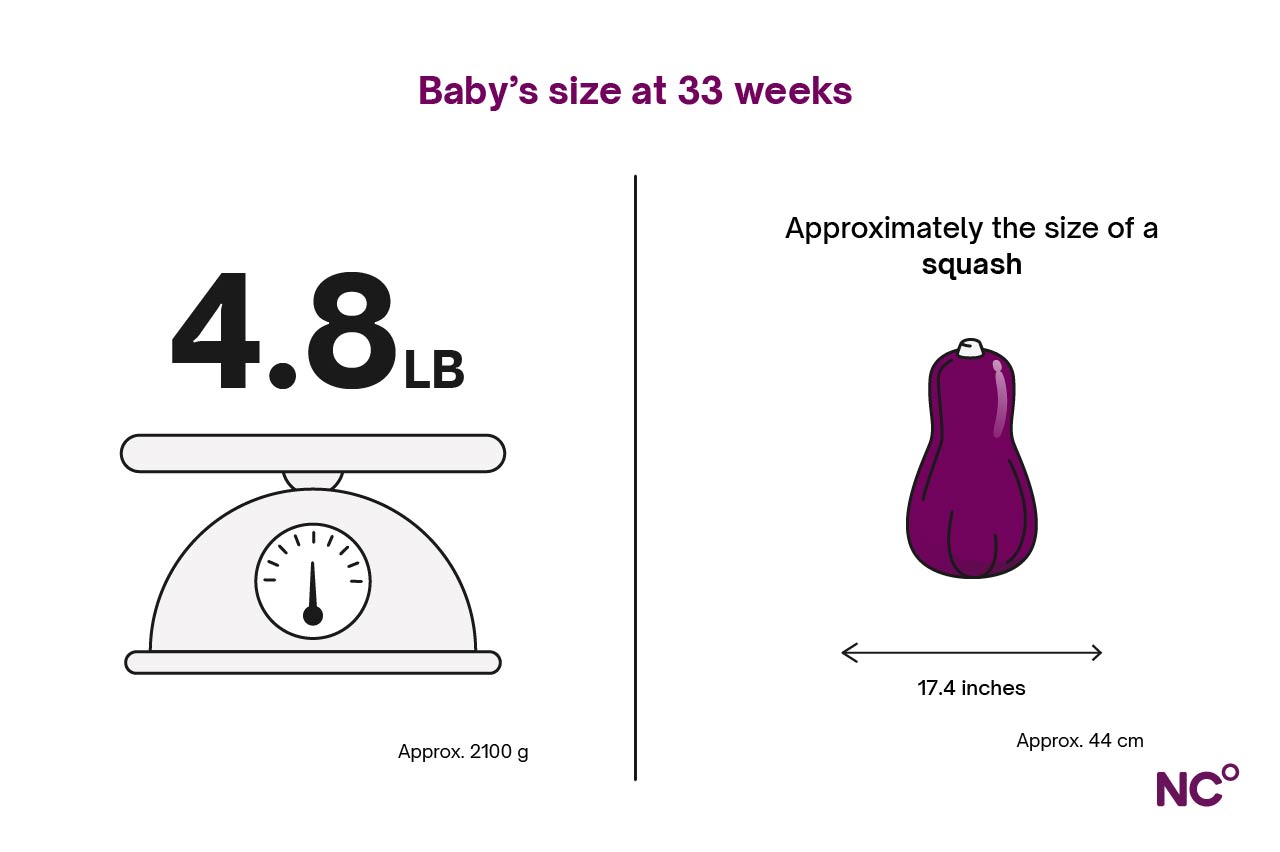
This week, your baby weighs between 4.5 to 5 pounds (2-2.3 kg) and is about 16.5 to 17.5 inches (42 to 44 centimeters) long [7]. This is around the size of a squash!
Pregnancy Symptoms during Week 33
Wrist pain
If you are experiencing aching or numbness in your fingers, hands, or wrists, it might be carpal tunnel syndrome brought on by pregnancy. Carpal tunnel is caused by the median nerve, which runs through your wrist and arm, being pressed. During pregnancy, swelling in your hands and wrists brought on by hormonal changes can make you more prone to experiencing carpal tunnel [8]. This is particularly true as swelling intensifies during the end of pregnancy.
If you are experiencing carpal tunnel, try to take breaks or avoid activities that worsen symptoms. You can also try wearing a wrist splint at night, available at pharmacies or online, but be advised that you likely have to wear it for 4 weeks before you will begin experiencing relief [8]. There are also various exercises, like wrist bends, lifts, flexes, and hand squeezes that can help provide pain relief and improve symptoms [9]. Hand and wrist issues usually resolve after birth for most women [10].
Urinary incontinence
Peeing your pants every time you laugh, cough or sneeze? This is referred to as stress urinary incontinence, or SUI, and is the most common type of urinary incontinence during pregnancy [11]. SUI can be experienced throughout pregnancy, or it can come in the final weeks as your growing baby puts more and more pressure on your bladder and pelvic floor muscles. Studies have also shown that hormones that loosen your ligaments and joints to make room for your growing baby and try to ease childbirth can also loosen the muscles that you use to help hold in your urine [11]. It is important to note that you can expect to experience some SUI in the weeks and months after you give birth, particularly if you have a vaginal delivery [10].
Check out our guide on strengthening your pelvic floor to learn more about your pelvic floor muscles and for recommendations on pelvic floor exercises that can help you with urinary incontinence during pregnancy and postpartum.
Swollen labia
Are you feeling new discomfort or pain in the area around your vagina and bottom? It could be swelling in your labia or perineum (the space between your anus and vagina). Weakening pelvic floor muscles and increased weight from your baby can put more and more pressure on your vagina. It is also possible that the veins in your vulva area can become large or swollen. This is known as vulvar varicosities, or varicose veins in your vulva, caused by increased blood volume and pressure in the vulva’s veins [12]. Hormone changes, increased blood flow, family history, and pressure on the veins in your pelvis can all cause swelling [12]. It is not uncommon to continue to experience vulvar varicosities or swelling of the labia postpartum.
For relief, you can try wearing maternity compression shorts or pantyhose designed to improve blood circulation [12]. It is also recommended to avoid standing or sitting for long periods of time [12]. Cold compresses, or ice packs with a cloth, can help with both pain relief and swelling [12]. Exercise, particularly pelvic floor exercises, can also help [12]. If you need further help managing pain and swelling caused by swollen labia or vulva varicosities, consider a consultation with a physiotherapist.
Tips in Week 33
- Start prepping a hospital bag: if this is your first baby, it is normal to overpack. And that’s OK! The most important thing when packing your hospital bag is trying to anticipate what will make you most comfortable, as well as what you will need to bring your baby home. This can include loose and comfortable outfits, nursing bras (if you are planning to breastfeed), heavy sanitary pads, extra underwear (comfortable underwear is recommended, maybe even some disposable underwear), chargers for phones and tablets, some healthy snacks, and some basic toiletries like toothbrush, toothpaste, and face wash. For your baby, you will need an outfit for them to go home in, plus a newborn hat, socks, and a car seat. The hospital or birthing center where you will give birth will likely have their own recommendations of what to pack, so be sure to check their website
- Stay cool: if you are progressing through your third trimester in the warmer weather months, it is important to keep hydrated and prevent getting overheated. Consider a plug-in air conditioning unit or battery-operated handheld fan to keep you cool. These can also be used at night to help you sleep!
- Creating a birth plan: as you learn about the facility where you will give birth, more about labor, and about different forms of pain relief during labor, you might consider making a list, or plan, of how you would want your birth to go. It is important to remember that a safe, healthy birth is priority number one, and that birth is ultimately unpredictable. Reasonable flexibility is a necessary part of any birth plan. However, it is important that you feel listened to and that you can request the things you need that will make you the most comfortable during birth. If you are planning to have a partner, family member, or friend in the delivery room with you, be sure to also share your plans and wishes with that person so they can support you during delivery.
- Consider birth control after pregnancy: though it might not be top of mind now, it is important to remember that you can get pregnant again within a matter of weeks after giving birth. You can talk with your partner already about what options might be best for you. In many cases, your doctor will talk to you about contraception before you leave the hospital after giving birth, so it is helpful to already have an idea of which options you are interested in.
- Remember those Kegel exercises: We’ve said it before, but we’ll say it again! Strengthening your pelvic floor muscles is important for supporting the pressure applied by your growing baby and helping with pelvic pain, urinary incontinence, and swollen labia. Strong and toned pelvic floor muscles can also help during delivery.
Following your pregnancy & beyond with Natural Cycles
Natural Cycles is the first FDA Cleared birth control app, offering a non-invasive and non-hormonal method for controlling your fertility. But did you know that Natural Cycles can support you during pregnancy and postpartum as well? NC° Follow Pregnancy will guide you through your pregnancy with weekly check-ins that tell you more about how your body and baby are developing. You can also use the app to track pregnancy symptoms and access the library of informative guides on various topics like sex, exercise, and eating during pregnancy. After giving birth, NC° Postpartum can help you recover from childbirth by offering tips and support on the various mental and physical changes you will experience. It’s quick and easy to switch modes in the app, meaning when you need to prevent pregnancy again you switch to using NC° Birth Control for a hormone-free contraceptive option.
Did you enjoy reading this article?



