41 Weeks pregnant: Baby development, symptoms and signs
Follows NC° Editorial Policy
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways
- Be on the lookout for labor signs — uncontrolled leaking might not be urinary incontinence, but rather your water breaking
- Indigestion and heartburn can be worse this week, but contact your doctor if you experience severe nausea or vomiting
- At week 41, your baby is considered overdue. While this is normal, and often no cause for concern, your doctor or midwife might talk to you about labor induction
Your due date has come and gone, and you have reached week 41 of your pregnancy. You might be thinking — when will this baby finally come out? Whatever the reason, your baby has decided to camp out a little bit longer. It’s normal to feel a mix of feelings like excitement, exhaustion, and stress in these final days of your pregnancy. In this article, we will talk about managing some symptoms you might be experiencing this week and check in on how your baby is doing. We will also discuss what it means to be overdue and cover labor induction. Finally, we will offer some tips on how to manage physically and mentally as you wait patiently (or impatiently) to meet your baby.
Your body at week 41
Frequent urination
At 41 weeks, your baby has likely moved farther down into your pelvis in preparation for birth. This can put even more pressure directly on your bladder, causing you to constantly feel like you need to go to the bathroom and making leaking worse. You can use panty liners or sanitary pads to help keep you comfortable and ease fears of leaking through underwear or pants. Continuing with those Kegel exercises, particularly at the end of pregnancy, can also ease leaking and help strengthen your pelvic floor in preparation for childbirth and postpartum recovery.
If you find you are leaking uncontrollably, or if the leakage is clear or pink-colored (and doesn’t smell like urine), this might be a sign that the membranes of your amniotic sack have ruptured. In other words, your water has broken! When your water breaks, the liquid can come out suddenly in a large rush, or it can trickle out more slowly. If you suspect that your water has broken, you should contact your birthing center or hospital immediately, even if you are not yet experiencing contractions.
Pelvic discomfort
As you get closer to labor, you might experience increased pressure in your pelvis. This can happen as your baby moves further down in your uterus in preparation for birth. You might also feel discomfort in your lower back and hips, even if you have not yet started having contractions. Increased pressure, pain, and discomfort could also be a sign that labor is beginning soon. Try to rest comfortably, using pillows for extra support. Also be sure to maintain good posture and equal weight between your legs when standing, sitting, and walking [1].
If the pain becomes severe, or if it is becoming impossible to get comfortable, contact your nurse, midwife, or doctor for advice.
Anxiety
Knowing you’re past your due date and that your baby can come at any time can take a toll on your mental health. Try to remember that around 5% of babies come on the exact day they are predicted to arrive, and that the calculation of due dates is not an exact science. While doctors still cannot determine with certainty why a baby passes its due date, research suggests genetic predisposition (hereditary trends that run in the family), as well as first births, can make it more likely for a baby to come late [2].
Though due dates, and the 40 week mark, can carry a great deal of emotional weight, being born after week 40 rarely harms the baby [2]. Your midwife or doctor will regularly check you and your baby’s health especially after you pass your due date, sometimes two or more times a week. This is to ensure that you and your baby are both healthy, that the placenta is still supporting your baby, and that there are no signs of infection for either of you [2].
While you wait for your baby to make its grand entrance, try to take some time to celebrate yourself and the tremendous job you have done growing your baby for 40+ weeks. Tired of responding to texts from family and friends asking “has the baby arrived yet”? If it helps, give yourself permission to take mental and physical space to be present and abstain from situations that will make you more stressed or anxious. As always, contact your healthcare team if you have any questions or concerns about your baby or your own health.
Nausea
Indigestion, heartburn, bloating and constipation can all contribute to feelings of nausea in your final weeks of pregnancy. Even if you have been suffering from these pregnancy symptoms for weeks, they can sometimes get worse at the very end of pregnancy, as your baby is at its largest [3]. Try to avoid eating large meals, eating before bedtime, and fatty or spicy foods, as these can make heartburn and indigestion worse.
If you experience sudden severe nausea and/or vomiting, contact your healthcare provider right away. Vomiting can be a sign of preeclampsia, a serious condition that requires medical attention. While doctors still do not know what exactly causes preeclampsia, it is widely understood as a hypertensive disorder (meaning related to high blood pressure) linked to issues with the placenta [4]. Preeclampsia can range from mild to severe, but requires immediate monitoring to prevent complications for both mother and baby.
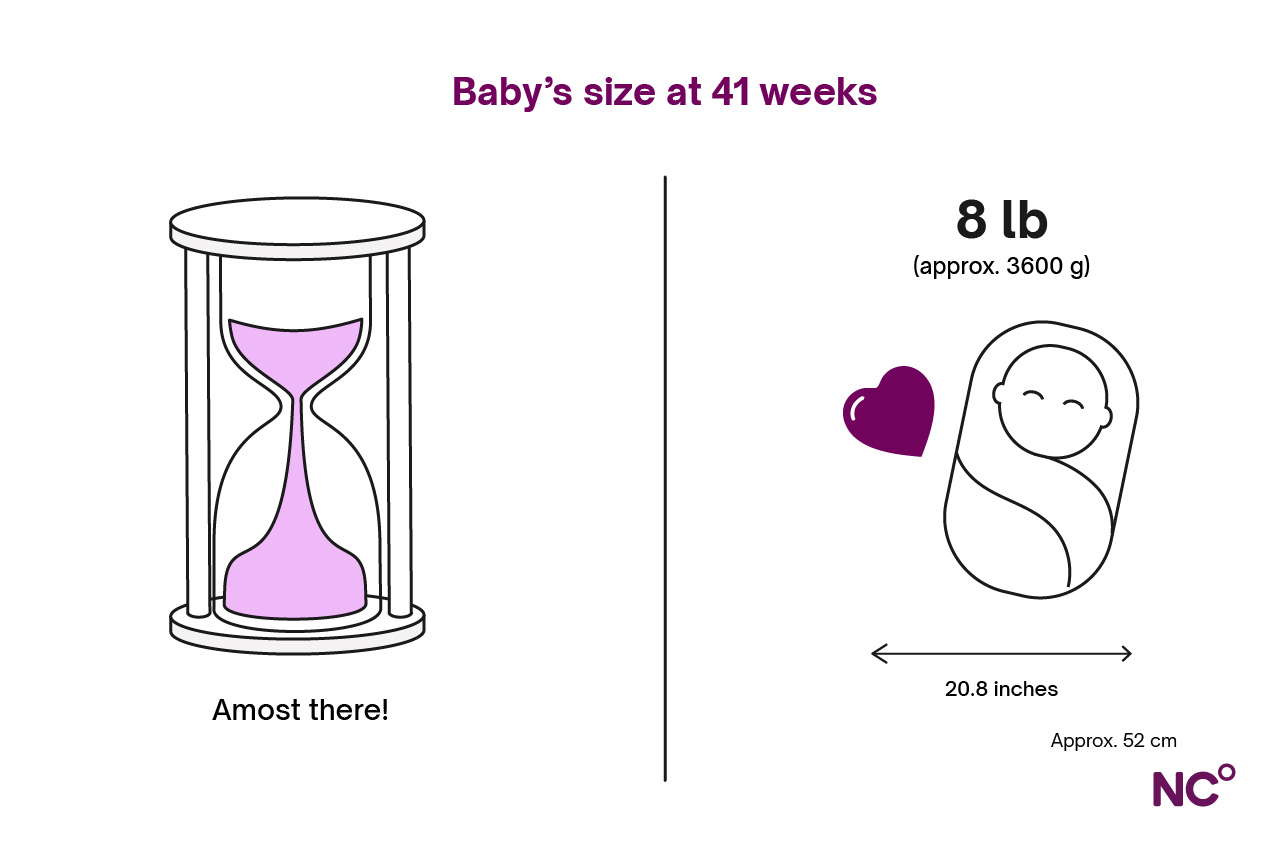
Your baby’s development at 41 weeks
Your baby is overdue - what are they doing in there? If your baby has settled in with no signs of wanting to leave the warmth of the uterus, they are most likely comfortably growing and gaining more fat with each passing day. At 41 weeks, all their organs and bodily systems are developed and ready for life outside of the uterus.
In your weekly, or likely more frequent, appointments with your nurse, midwife or doctor, they will monitor you and your baby’s health for any signs of distress. This can include a non-stress test to measure the baby’s heart rate and/or an ultrasound to check your baby’s heart rate, breathing, movement, and size. In addition to general health and condition, your healthcare team is also checking that your baby is not getting too big for a safe vaginal delivery and that there is still enough amniotic fluid in your uterus. Your doctor or midwife might also perform an internal exam to check if your cervix has begun softening or opening.
Natural labor and induced labor 41 weeks
Most medical professionals try to wait for labor to begin naturally [5]. This means that your body will begin having contractions on its own, you will discharge your mucus plug, and your water will break (sometimes before contractions start, sometimes after). You might have the signs of labor seared into your memory at this point, but here’s a recap:
- Contractions: these are the most universal and easily observable sign of labor. Labor contractions can start off mild, but will come at regularly timed intervals and get stronger and closer together.
- Mucus plug: this is the mucus that sits in the mouth of the cervix and is released before or during labor. It might be hard to distinguish from vaginal discharge, but your mucus plug is generally thicker than other vaginal discharge and can have red, brown, or pink blood in it.
- Rupture of membranes, or breaking water: this is when your amniotic sack opens, releasing the liquid inside. It can come in a sudden gush or can leak out slowly and steadily. Your water can break before you start experiencing contractions, or more commonly, after. If you experience an uncontrollable leak, or you notice leaking fluid that is clear or slightly pink in color, contact your healthcare team right away because only they can determine if it is amniotic fluid.
At 41 weeks pregnant, your healthcare team can suggest artificially, or medically, inducing labor. While being overdue is generally considered safe, depending on the age, weight, and health conditions of the mother alongside the condition of the baby, your doctor or midwife might decide that it is time to medically help start labor. In most cases, doctors will not let pregnancies continue past 42 weeks.
There are generally two approaches to labor induction, ripening the cervix and inducing contractions. Let’s take a closer look at both:
- Ripening the cervix: during labor, your cervix narrows and opens (or dilates) so that the baby can come out. The hormone prostaglandin can also be used to help soften and open the cervix [6]. Doctors or midwives can also use a small balloon, called a catheter, or a sponge, known as an osmotic dilator, to help open the cervix.
- Starting contractions: in order to get your uterus to start having contractions, the hormone prostaglandin can be administered as a tablet or gel in your vagina, as oral medication, or the hormone oxytocin can be administered through an IV.
It is possible during induction that your water will also be broken by a midwife or doctor. This is known as the artificial rupture of membranes, or AROM.
Labor induction is considered safe and is very common, used in approximately a quarter of births in high-income countries [5]. However, having an induction usually requires you to give birth at a medical center or hospital. Inductions can also be more painful than labor that begins naturally [8].
Remember that having an induction does not limit your pain relief options in any way, so be sure to communicate constantly with your healthcare team if you need pain relief during induced labor. It is also important to know that inductions do not always work. In some cases, babies will need to be born via caesarian section (or c-section).
Tips in week 41
- Consider putting down the phone: whether it’s friends and family eagerly awaiting news of your baby’s arrival or social media constantly feeding you pictures of births and babies, consider taking a little break from technology. But don’t let the phone get too far away, remember that labor can begin at any time and you’ll want to make sure you can track your contractions and call your birthing or maternity center when the time comes.
- Remember, there is no proven way of starting labor on your own: you might have heard or read about certain methods for starting labor. Unfortunately, there is no medical or scientific evidence that any of these methods work and in some cases, they can be harmful to you or your baby.
- Treat yourself: whether it is a mani-pedi (avoiding gel or acrylic), some takeout, or a (pregnancy-safe) massage, treat yourself this week. You deserve it!
- Double-check your hospital plan: make sure you know the right phone numbers of doctors or hospitals to call, the phone tree of who to inform when you go into labor, how you’re getting to the hospital, and who is responsible for caring for other children and pets. This can help put your mind at ease as you wait for labor to begin.
- Pack some extra snacks or entertainment: induced labor can sometimes take longer than natural labor. Consider adding some extra snacks or entertainment to your hospital bag, just in case.
Natural Cycles after giving birth
Did you know that Natural Cycles, the first FDA Cleared birth control app, can also support your recovery after birth and beyond? NC° Postpartum offers access to resources and guides for your mental and physical help after childbirth and during your transition to motherhood. When your fertility returns, NC° Birth Control is a great option for non-invasive, hormone-free birth control tailored to you. Find out how Natural Cycles can support you, today.
Did you enjoy reading this article?



