Perimenopause joint pain: Causes, symptoms, and how to treat
Follows NC° Editorial Policy
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- Joint pain is a surprisingly common symptom of perimenopause, with an average of about 70% of women experiencing it during this transitional life stage
- Your body goes through a lot during perimenopause, including muscle loss, weight gain, and hormonal changes — all of this can put extra strain on your joints
- There are plenty of remedies available to help soothe joint pain but be sure to chat with your healthcare provider to find the best treatment option for your body
When thinking about menopause and perimenopause, we usually associate it with symptoms like hot flashes and irregular periods. But did you know that joint pain is one of the most commonly reported symptoms of perimenopause? Across various studies, musculoskeletal pain has been reported by 50 to 89% of perimenopausal women [1]. If you’re feeling that stiff, achy feeling in your joints during this stage of life, you’re not alone.
Perimenopause joint pain can make everyday activities difficult to manage, so it’s important to understand why this happens and what you can do about it. In this article, we’ll answer the question, “does menopause cause joint pain?” along with the causes, symptoms, and available treatments for any perimenopause joint pain you may be experiencing.
Why do we get joint pain during menopause?
Joint pain is a common symptom many of us will experience after menopause and in the years prior. You may have heard or used the term “menopause” to refer to the time in our lives when we near the stop of our menstrual periods, but this time period is actually called “perimenopause.” The term “menopause” refers to the point at which we haven’t had a period or any bleeding in one full year, after which we become postmenopausal [2].
Perimenopause is characterized by irregular hormonal fluctuations of the female sex hormones estrogen and progesterone in your body. As these hormones fluctuate irregularly, they also gradually decline over time until menopause, at which point levels are very low [3, 4].
These fluctuations, particularly with estrogen, may be related to the symptoms associated with perimenopause, including joint pain and bone density loss. Estrogen contributes to many bodily processes that maintain bone and cartilage health, so the gradual decline of estrogen over the course of perimenopause may be the underlying cause of joint pain, although more comprehensive studies are needed to confirm that link [3, 4, 5].
Is joint pain linked to perimenopause?
So yes, while joint pain can be linked to perimenopause, it may not necessarily be the underlying cause. Many other factors like weight, physical activity, genetics, and more can cause chronic conditions like arthritis or temporary injuries, all of which can also be the cause of joint pain.
But if you’ve consulted with your healthcare provider and it seems like the joint pain is directly linked to perimenopause, know that this is a normal part of the aging process. The good news is that there are quite a few treatment methods available to help you navigate this transition (more on that later).
What causes joint pain during perimenopause?
Perimenopause comes with a host of symptoms including menstrual irregularity, hot flashes, trouble sleeping, mood changes, and yes, joint and muscle discomfort [2]. You might also notice a gradual loss of muscle mass and strength throughout perimenopause and into postmenopause [3]. It’s common to gain some weight as well, since the body starts to use energy differently and your hunger signals might change during perimenopause [2, 5]. Both of these factors — muscle loss and weight gain — could put extra strain on your joints, causing discomfort or outright pain.
It’s important to remember that while uncomfortable symptoms are a common feature of perimenopause, that doesn’t mean you should just “get on with it.” Help is available and it’s worth connecting with your healthcare provider — particularly if your symptoms start to get in the way of your everyday life.
What else causes joint pain?
As we mentioned earlier, perimenopause and the hormonal shifts associated with this life stage may not be the direct cause of your joint pain. It’s very possible that another condition is causing your joint pain. Some common joint pain sources include:
- A muscle sprain or strain [6]
- Chronic conditions like inflammatory arthritis or fibromyalgia [7, 8]
- Tendonitis or tendinosis, meaning pain in tendons rather than specific joints or muscles [9]
Each of these does require separate medical attention and treatment and may not be associated with the hormonal fluctuations of perimenopause, although one condition could be exacerbating the other. It’s a good idea to reach out to your healthcare professional and talk about your symptoms and history. This can help you pinpoint the root cause of the pain so that you can find the right treatment for lasting relief.
How to treat joint pain caused by perimenopause
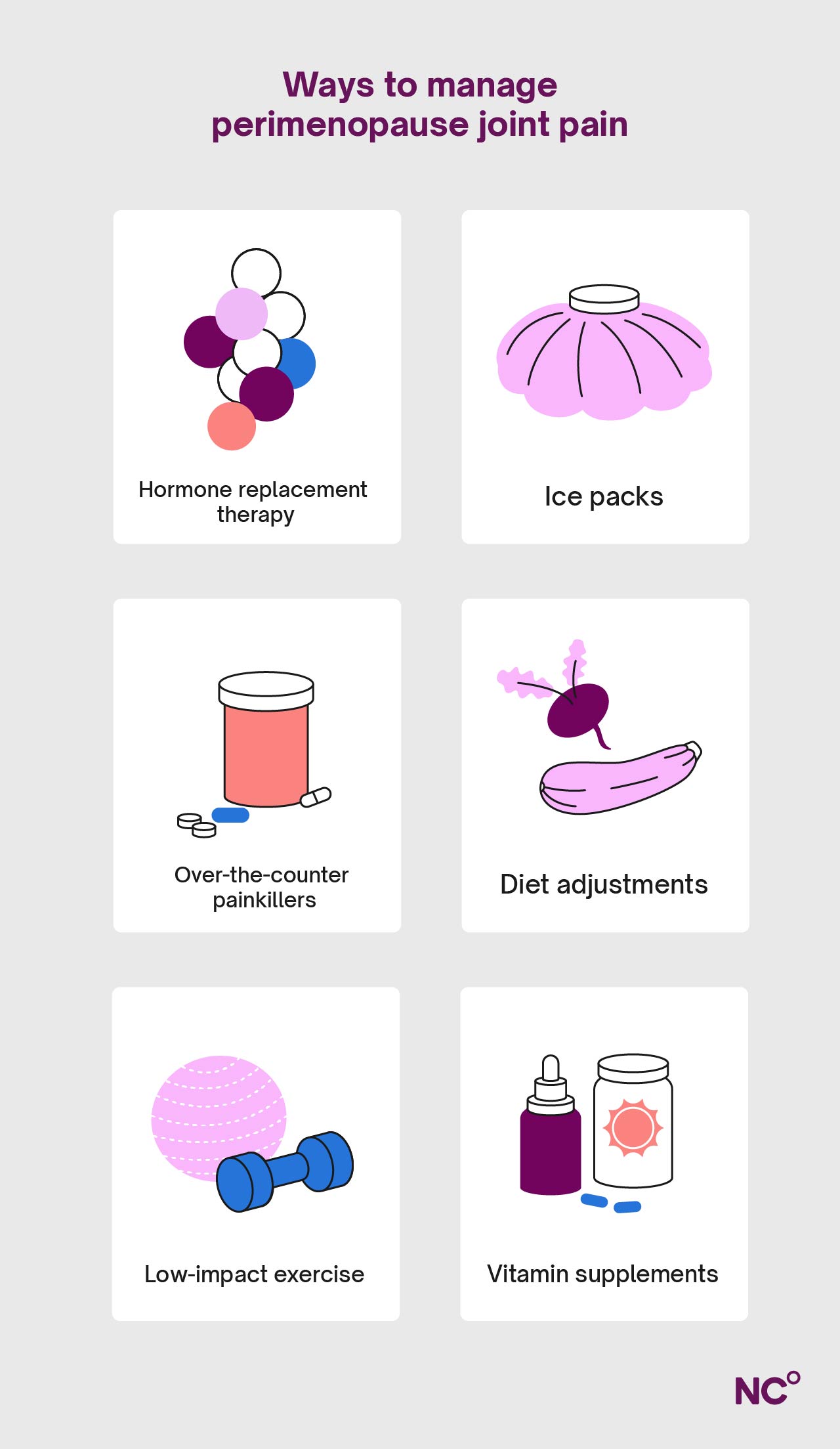
When speaking with your healthcare provider, they may recommend one or a combination of some of the treatments outlined below. Remember that each one may not work in the same way for everyone, so you may have to try a few to find the right one for your body. Let’s go through a few in detail:
Ice packs: For at-home, immediate relief of the joint pain associated with perimenopause, try temperature therapy in the form of an ice pack. Joint pain is often associated with inflammation, so applying a cold compress for about 20 minutes can provide relief and help increase mobility [10].
Over-the-counter (OTC) painkillers: At OTC doses, medications like ibuprofen (U.S. brand name: Advil), acetaminophen/paracetamol (Tylenol), and naproxen sodium (Aleve) can relieve mild to moderate joint pain associated with perimenopause, or many other types of joint pain you may be experiencing. At higher prescription doses, they can also help reduce inflammation. Consult with your healthcare provider for more information on which dose would be best for your case. [11]
Diet adjustments: A healthy diet can help prevent the development of chronic conditions like osteoarthritis, and might also make it easier to tolerate the symptoms of an existing condition. Eating lots of fruits and vegetables, or even following a plan like the Mediterranean diet, can help you manage your weight and the symptoms associated with perimenopause more effectively. It’s also a good idea to lower your salt and alcohol intake while you’re making these adjustments. [12].
Low-impact exercise: Gentle, regular physical activity (such as walking, yoga, and light strength training) can help alleviate some of the joint pain and other symptoms associated with perimenopause as well. It can also contribute to higher quality sleep, elevate your mood, and reduce the risk of injuries. Just remember to keep the exercise at light to moderate levels and listen to your body throughout the workout [13].
Sleep: Disrupted sleep patterns are common during perimenopause, and a poor sleep schedule can have quite an impact on your daily physical and mental health. Sleep plays a role in metabolism, nutrient absorption, and more, so it’s important to prioritize when your body is undergoing the perimenopause transition. Healthy sleep can lead to healthy muscles, healthy bones, and a healthier body overall [12].
Hormone replacement therapy: Since joint pain may be related to the decrease in estrogen that happens over time during perimenopause, hormone replacement therapy (HRT, also known as menopausal hormone therapy or MHT) might help ease the symptoms. While there are many methods of HRT, it usually involves taking a daily pill, patch, or spray [14].
HRT may not always work the same way for everyone, but the research thus far is promising. The estrogen decline during perimenopause can lead to five primary changes, all of which can result in joint pain:
- Increased inflammation
- Decreased bone mineral density
- Arthritis
- Sarcopenia (a loss of muscle mass and strength)
- Fewer muscle stem cells
Replacing the lost estrogen with supplementation in the form of HRT or MHT can ease these effects, leading to less inflammation and better musculoskeletal function overall. This also means there is a lower chance of developing further sarcopenia, arthritis, and osteoporosis into postmenopause [14]. Be sure to speak with your healthcare professional about the risks, benefits, and course of treatment before making a decision about hormone therapy.
Vitamin supplements: Getting the right amount of minerals like vitamin D and calcium can support bone and joint health. These are found in foods like egg yolks and dairy products, but they can also be found in the vitamin aisle at your local pharmacy. We’ll dive into a few more supplements that may help with joint pain below, but make sure to talk to your healthcare provider about recommended doses if you’d like to start taking supplements [14, 15].
Can supplements help with perimenopause joint pain?
Aside from calcium and vitamin D, supplements like magnesium and collagen can also help strengthen your body and ease joint pain.
Limited studies have shown that increasing magnesium intake either by diet changes (leafy greens, legumes, nuts, and whole grains) or with supplements can help increase bone density in postmenopausal women. Some of its functions in the body include energy production, bone development, and the transport of calcium across cell membranes [15].
Collagen is also an essential nutrient that can be taken as a supplement. It contributes to cartilage health, and has been shown to have a positive effect on bone strength and mineral density when taken consistently over time [16].
Again, it’s worthwhile consulting a healthcare professional before you start making any sort of major dietary or supplement adjustments. They can provide the best personalized guidance to make sure you’re on the path to perimenopause joint pain relief.
When to see a doctor about perimenopause joint pain
As we’ve mentioned throughout this article, it’s a good idea to talk to your doctor about any sort of pain you’re experiencing, particularly joint pain that makes everyday activities difficult. There are many underlying causes for joint pain, including perimenopause, and understanding that root cause can help you get effective treatment.
We do want to note that if you have severe, sudden joint pain, especially in one joint, that’s associated with swelling or the skin color changing, that may indicate an injury that needs urgent medical attention. If these symptoms are associated with shivers or a fever, this may indicate an infection that also needs immediate medical attention [17].
Most of the time however, joint pain is just a normal part of the aging process. Luckily, there are many remedies and treatments available to help keep you moving through perimenopause and beyond.
Learn more about your perimenopause journey with Natural Cycles
Tracking your cycles and symptoms over time with a tool like Natural Cycles can help you and your healthcare provider have informed conversations about the pain you’re experiencing and the right treatments. Natural Cycles is more than just a tracker though — it provides learning resources, community, and uses science-backed technology to give you deeper insight into your body. See if Natural Cycles is right for you today.
Did you enjoy reading this article?



