Period blood clots: What are they, causes & are they normal?
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key takeaways:
- It’s common to have some blood clots during your period, which are made up of coagulated blood and tissue from the uterine wall
- Blood clots that are larger than a quarter are a sign of a heavy period, and because large clots can also be a symptom of an underlying condition, you should speak to your doctor if they happen frequently
- Treatment options for heavy periods include tranexamic acid, hormonal birth control, iron supplements, and surgery
Most of us have probably noticed blood clots at some point during our periods. They may look like small chunks of dried-up blood, or you may have spotted jelly-like blood clots mixed in with your period blood. While this might feel alarming at first, clots are actually natural and in most cases, they’re nothing to worry about. In this article, we’ll dive into what causes blood clots during your period, when to reach out to your doctor about it, and treatment options for heavy periods.
What are period blood clots?
During each menstrual cycle, the uterine lining thickens to prepare for the implantation of a fertilized egg cell. If implantation doesn’t happen, the uterine lining sheds in the form of a bleed — your period [1].
Blood clots don’t just happen during periods. They are the body’s natural response to bleeding, regardless of where in the body it happens. The clotting process — when the blood coagulates — starts whenever there’s an injury that involves a bleed. Small blood cells called platelets start clumping together and a kind of protein, fibrin, forms a sticky mesh that the platelets and red blood cells attach to [2]. The result is a blood clot that works sort of like a plug to help stop the bleeding — if the bleeding is caused by a cut or scrape, you’ll soon have a scab covering the wound.
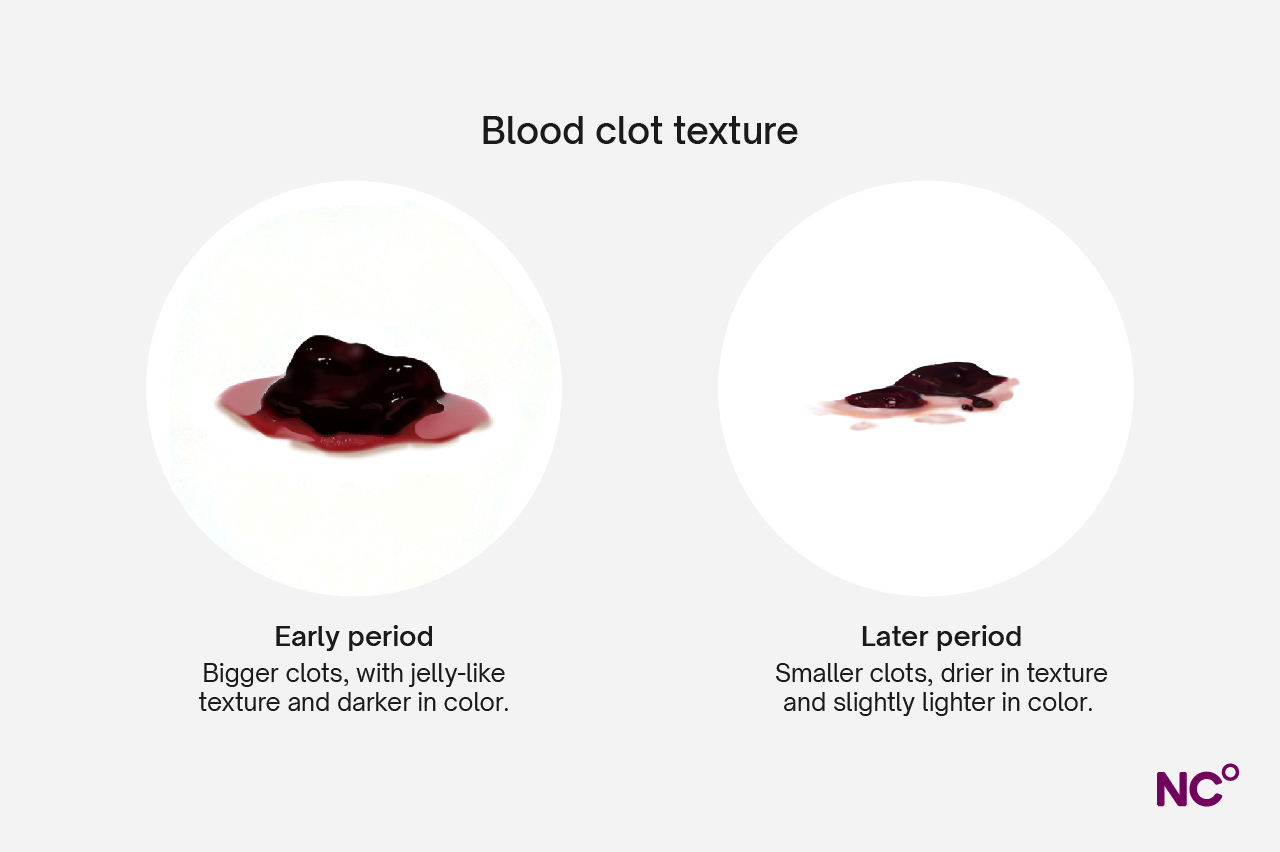
So, what does this have to do with periods? Well, period clots essentially work in the same way, even though the clots don’t end up plugging the source of the bleed. Blood that sits in the uterus, cervix, or vagina will naturally start to coagulate and clots are formed, which then come out during the period bleed [3]. Sometimes, the coagulated blood will be mixed with tissue from the uterine wall, which is why you may also see jelly-like blood clots during your period.
Is it normal to have blood clots during my period?
It’s normal that your period contains some clots, and you’ll usually see them during the first few days when your flow is heavier. Every person is unique and will have their own bleeding pattern during their period. Some have more period clots, while others barely have any. As well as varying from person to person, it can also vary from one period to the next. So sometimes you might get lots of clots, and some periods hardly any. However, it’s good to keep an eye on what a typical period bleed looks like for you — passing large clots may be a sign of something more serious if it happens often.
What do normal period clots look like?
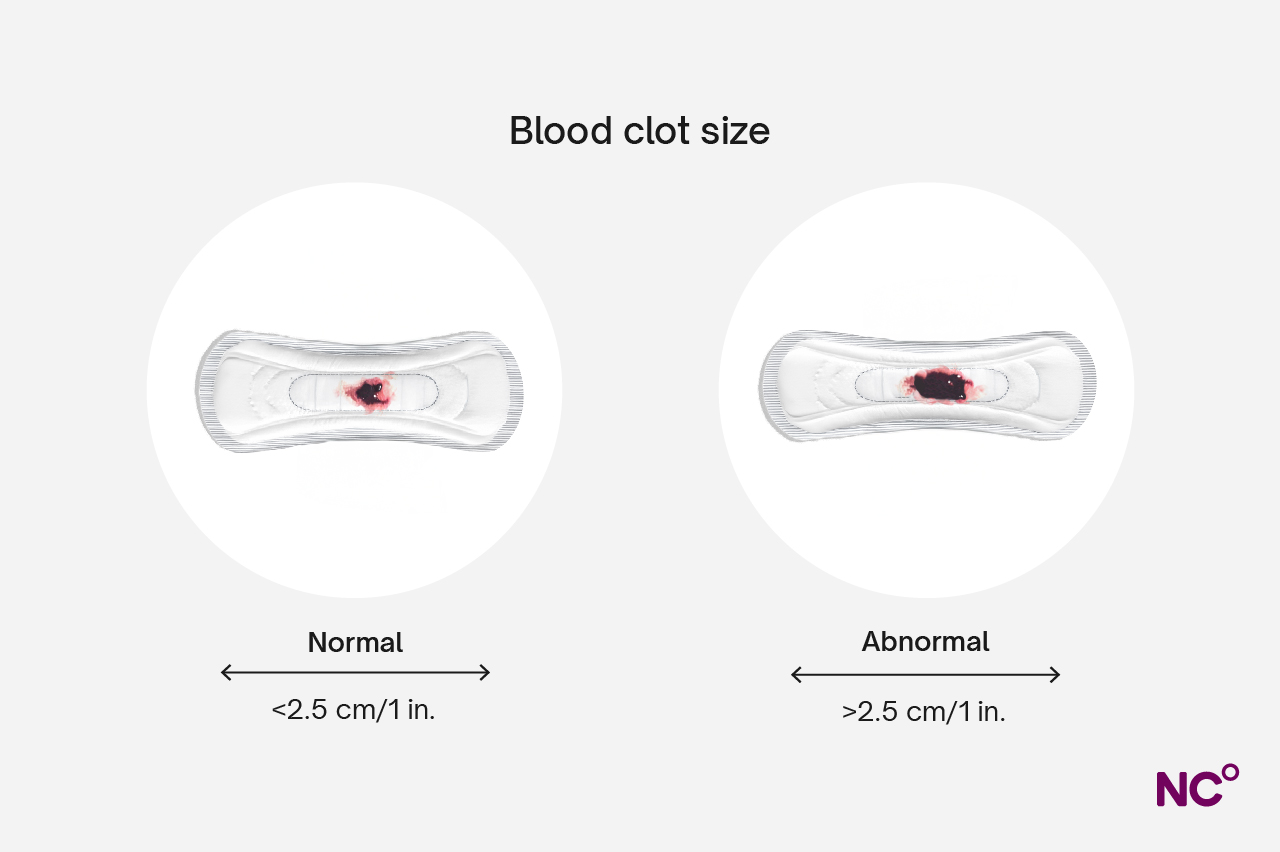
Period blood clots are considered normal if they are smaller than a quarter (about 1 inch or 2.5 cm) in size. They can vary a bit in their appearance but will usually look like clumps of dried blood, and the color can vary from red to dark brown depending on how old the clot is. You may also notice that your clots have a jelly-like consistency if the blood is mixed with uterine tissue.
What are abnormal period clots?
Period blood clots may be considered abnormal depending on how frequent and how large they are. Clots that are bigger than a quarter in size are considered abnormal, especially if they happen often. This can either mean that you have several large clots during the course of one period or that you notice them over the course of several periods in a row.
Larger clots tend to happen during the days when your flow is heavier (similar to small clots), but large clots are also a sign of heavy periods in itself. An average period bleed is about 2-3 tablespoons, but you may lose double the amount of blood during a heavy period [4]. It’s always a good idea to speak with your doctor if you think your periods are heavy.
What does period blood look like?
Now that we’ve talked about how to spot a period clot, let’s turn our attention back to periods more generally. The appearance of the blood typically changes a bit during the course of a period, and it can also change from one period to the next. Jelly-like tissue from the uterine lining can also affect how it looks.
When it comes to the color of period blood, this is often an indication of how old the blood is. Blood becomes darker and turns brown when it’s exposed to oxygen (think of a blood stain on clothing when it dries). That’s why you might see darker red or brown blood at the beginning and end of your period — when the flow isn’t as heavy, the blood sits in the uterus or vagina for longer before it comes out and is exposed to oxygen during that time. When the flow is heavier, you’ll typically see brighter red blood which indicates that it’s fresher.
It’s always good to speak with a healthcare professional if you have questions about how your period blood looks. You should also reach out if you notice unusual discharge colors like your blood appearing orange or gray, or if it has a foul smell, since this can be an indication of infection. Here’s a breakdown of the different colors of period blood and discharge and what they mean:
- Bright red: fresh period blood, usually happens during the middle of the period
- Dark red: older blood that has oxidized, often at the start or end of the period. Can also happen after pregnancy or during postpartum bleeding.
- Brown: older blood that has oxidized, often at the start or end of your period. Can also happen during postpartum bleeding or perimenopause.
- Black: Oxidized older period blood. Can also be a sign of infection, something blocking the vagina, miscarriage, or postpartum bleeding.
- Pink: blood mixed with cervical mucus. Can happen during perimenopause or indicate lower estrogen levels.
- Orange: blood mixed with cervical mucus, can indicate infection.
- Gray: can indicate infection.
- Yellow: blood mixed with cervical mucus, but can indicate an infection if coupled with other symptoms, like pelvic pain.
- Green: can be a sign of infection, such as a sexually transmitted infection (STI) or urinary tract infection (UTI).
What causes large blood clots during my period?
Large blood clots are a sign of heavy periods. Everyone has their own unique period characteristics and heavy bleeding doesn’t necessarily mean that there’s anything to worry about. However, it’s always good to check with your healthcare provider if you’re experiencing heavy periods that interfere with your daily life.
There are some potential causes of heavy periods that are good the be aware of, such as:
- Endometriosis: A condition that causes tissue similar to the uterine lining to grow outside of the uterus. Heavy and painful periods, often coupled with large period clots, are a common symptom of endometriosis.
- Adenomyosis: This condition causes the uterine lining to grow into the muscles of the uterus, which can both be painful and lead to heavy periods [5].
- Polycystic ovary syndrome (PCOS): PCOS is a condition that affects hormones, and this often leads to irregular menstrual cycles. Heavy periods can also be a symptom for some people.
- Fibroids: Fibroids are noncancerous growths that can form in the uterus, and they may lead to irregular periods or heavy bleeding. While fibroids are usually harmless, they should be checked out by a healthcare professional to make sure there are no other health concerns.
- Certain types of birth control: The copper IUD can impact the menstrual cycle by causing heavier, and sometimes longer, periods. Hormonal birth control methods, such as the birth control shot or mini pill, may also cause heavy bleeding for some people.
- Thyroid conditions: Hypothyroidism is a condition where the body isn’t producing enough thyroid hormone, which can affect the menstrual cycle and lead to irregular and heavier periods.
- Certain types of cancer: While rare, heavy bleeding can be an early symptom of endometrial cancer.
- Pelvic inflammatory disease (PID): PID is an infection in the female reproductive system, which can cause heavy periods along with other symptoms like pain in the lower belly or pelvis, smelly discharge, and pain during sex.
- Certain medications: Some medicines like, for example blood thinners and aspirin, can lead to heavier bleeding since it prevents the blood from coagulating as normal. Make sure to check with your doctor before starting a new medication if you already have heavy periods.
- Bleeding disorders: Bleeding disorders are rare conditions that affect the blood’s ability to coagulate. Heavy periods are one sign, but you’ll likely also notice other symptoms like nosebleeds, that you bruise easily, or that you bleed for longer than others after injuries. The most common bleeding disorder is called von Willebrand Disease [6].
- Miscarriage or abortion: A pregnancy loss or termination can result in heavier bleeding than a regular period.
[7, 8, 9]
When to see a doctor
Because heavy bleeding during your period can be a sign of an underlying condition, it’s always good to speak with your healthcare provider to see if there’s anything more going on if you notice heavy or abnormal bleeding during your cycle. Even if it’s not caused by anything specific, your doctor can help explore what options are available for you to relieve or manage symptoms.
You should always reach out to your doctor if:
- You need to change tampons or pads every 1 to 2 hours, or need to change them during the night
- You need to wear more than one pad at a time
- You have large blood clots in your period (bigger than a quarter)
- Your period lasts for more than 7 days
- Your period disrupts your life or prevents you from taking part in activities you enjoy
- You have severe pain during your periods
[10, 7]
If your flow is heavy, it’s also possible to develop anemia, which is when your body doesn’t have enough red blood cells to efficiently transport oxygen [11]. This might make you feel tired, dizzy, or short of breath.
How are heavy periods diagnosed?
Because the causes of heavy periods are so varied, it’s important to understand if there’s an underlying condition before deciding on a treatment plan. The first thing you can expect when you visit your doctor is that they will ask about your medical history. For example, you should be prepared to tell them about what your periods are usually like, if you have any other symptoms, take any medication, or have a family history of conditions that might be related to heavy periods.
Next, they will likely do a pelvic exam — this is a typical gynecological exam where your doctor examines your pelvic area — before deciding if more tests are needed. Depending on what they suspect might be causing your heavy periods, they may suggest doing one or a couple of the following:
- Imaging tests: An ultrasound or MRI (magnetic resonance imaging) scan can be done to look at your internal organs.
- Sonohysterogram: A special kind of ultrasound which is done when fluid is injected into the uterus, which allows your doctor to spot issues with the uterine wall.
- Pap smear: This test involves taking a small sample of your cervix to check for signs of infection or cell abnormalities.
- Blood tests: Blood tests can be used to check hormone levels, for example, to see if your thyroid is working as it should or if you have any hormonal imbalances that could cause heavy periods.
- Endometrial biopsy: A small sample is taken from the uterine wall, which is then examined under a microscope to look for abnormal cells. This test can be used to diagnose fibroids, infection, or endometrial cancer.
- Hysteroscopy: During this procedure, a small tube with a camera is inserted into the uterus through the cervix. This allows your doctor to look inside your uterus and can be used to check for fibroids or other abnormalities.
While these processes and procedures may sound daunting, the first step is to talk to your doctor. They will be able to advise on the right diagnostic method for your particular situation and support you in getting the right information and treatment you need.
[7, 4]
How to treat heavy periods
There are several different treatment options available for heavy periods, and again, it will depend on what the underlying cause is. In most cases, the first step to treat heavy period bleeds is medication, but surgery can also be considered if other treatment options don't work.
Medications for heavy periods
When it comes to medicine, there are a few that have been shown to be effective for heavy periods. Make sure you speak with your healthcare provider to find which would work best for your situation.
- Tranexamic acid: Tranexamic acid, such as Lysteda, is a type of medication that improves the body’s blood clotting ability. You’ll usually take it during your period to reduce the bleeding. [12]
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen or Naproxen, can help with both heavy bleeding and painful period cramps. You can get these over the counter, but it’s best to check with your doctor first since these medicines can increase bleeding for some people.
- Hormonal birth control: A long-term treatment you can consider if you have heavy periods that are caused by endometriosis, PCOS, or fibroids. The hormonal IUD has been found to effectively reduce heavy bleeding [13], but there are many options available depending on your needs.
- Gonadotropin-releasing hormone agonists: A type of medication used to treat heavy periods caused by fibroids. They work by reducing the size of fibroids and also stop the menstrual cycle. However, this is only a short-term treatment that can be used for a maximum of six months due to the increased risk of certain side effects with long-term use, and the effect goes away once it’s stopped.
- Iron supplements: If you have anemia, you’ll usually be prescribed iron supplements to help replenish the iron levels in your blood.
[7, 4]
Surgery to treat heavy periods
There are also some surgical options that can be used to treat a heavy flow if medications don’t have the desired effect, for example:
- Dilation and curettage (D&C): This is a procedure where some of the uterine lining is removed, which can help reduce bleeding during your period.
- Surgery to remove fibroids: There are a couple of different surgical options for uterine fibroids. During a myomectomy, the surgeon removes fibroids in the uterus (often by a hysteroscopy, a kind of tube that is inserted through the cervix). A uterine artery embolization (UAE) is another type of procedure that stops fibroids from growing by blocking off their blood supply.
- Endometrial ablation: This is a procedure where the uterine lining is destroyed, which reduces or stops periods altogether. It’s usually not possible to get pregnant after having this procedure, but it’s still important to use birth control afterward since there’s a risk of serious complications if you were to get pregnant.
- Hysterectomy: A hysterectomy is a surgery to remove the uterus, and this is usually used as a last resort if other treatments haven’t worked.
[7, 4]
Get to know your body with Natural Cycles
Periods are still surrounded by a lot of stigma. Here at Natural Cycles, we believe that everyone should have the information they need to take charge of their own health — and that includes knowing what your period looks like. The NC° app allows you to keep track of your periods, including how long they last, the heaviness of your flow, as well as any pain you experience so that you can easily spot patterns over time.
Whether you’re looking for a non-hormonal birth control option, are ready to start a family, or just want to learn more about your body: why not check out if Natural Cycles could be right for you today?
Did you enjoy reading this article?
