Birth control effectiveness: Different types & chart
Follows NC° Editorial Policy
At Natural Cycles, our mission is to empower you with the knowledge you need to take charge of your health. At Cycle Matters, we create fact-checked, expert-written content that tackles these topics in a compassionate and accessible way. Read more...
Key Takeaways:
- No birth control is 100% effective. Whatever method you choose to use, there will still be a risk of pregnancy
- However, some birth control methods are more effective than others, and the good news is that using birth control can significantly reduce the risk of getting pregnant
How can we measure birth control effectiveness?
Every one of us is different and will have a different experience with birth control. However, it’s important we have a clinical measurement when we talk about birth control effectiveness so we can understand how well a method works for a larger number of people. In the contraceptive landscape, we normally talk about two measures of effectiveness called typical use and perfect use [1].
What is typical use?
Typical use reflects how birth control is used by real people in real life. As well as method failure, typical use also incorporates user error. This includes [1]:
- The method being correctly used every time the couple have sex
- The method is correctly used, but not used every time a couple has sex
- The method is used, but sometimes incorrectly
- The method is used incorrectly or is forgotten to be used
As you can see, typical use provides room for error - hence why the failure rate is usually higher than perfect use. This is particularly true for methods that require work from the user, for example, male condoms have a typical use of birth control effectiveness of 87% [2].
What is the perfect use?
Without taking into account user error, perfect use looks at the method’s effectiveness in a perfect world — i.e. if it was used exactly as it was intended every time a couple had sex. There is still a failure rate that applies if the method itself should stop working, but perfect use tends to be higher than typical use as it removes user error completely. For example, male condoms have a perfect use effectiveness of 98% [2].
What is the Pearl Index?
The Pearl Index is defined as the number of pregnancies that would happen for one method per 100 women over a year. So for example, the birth control pill has a typical use effectiveness of 93% and a Pearl Index of 7. So that means that we expect seven women in one year will get pregnant from using the pill. The pearl index is easy to calculate and understand, and it can be computed for both typical use and perfect use.
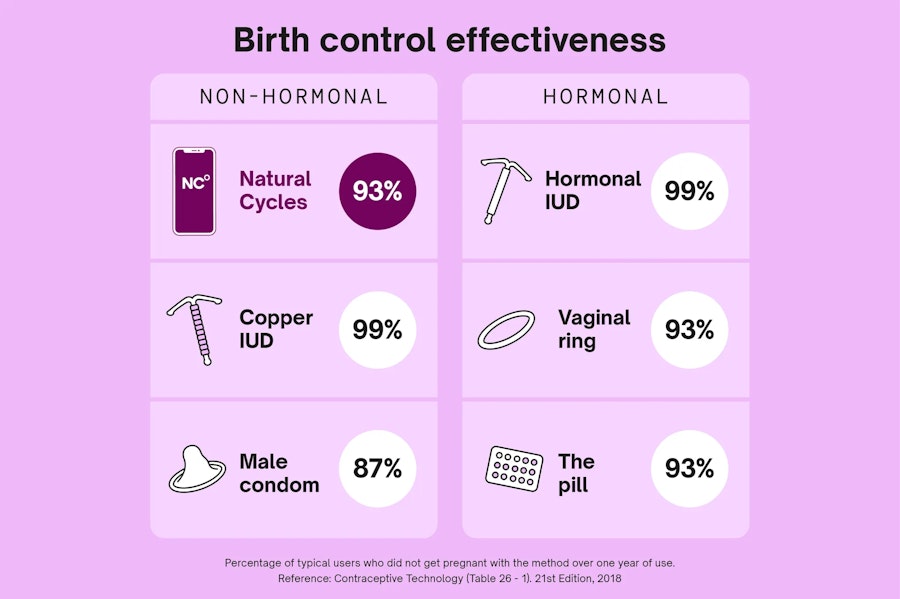
Birth control effectiveness chart
Since every method is different and works in its own way, the effectiveness of methods can vary quite considerably. It’s worth knowing the effectiveness of different methods to understand how effective your method is in the wider contraceptive landscape. Below is a table of birth control effectiveness showing both typical use and perfect use for a range of common methods including both hormonal and non-hormonal birth control.
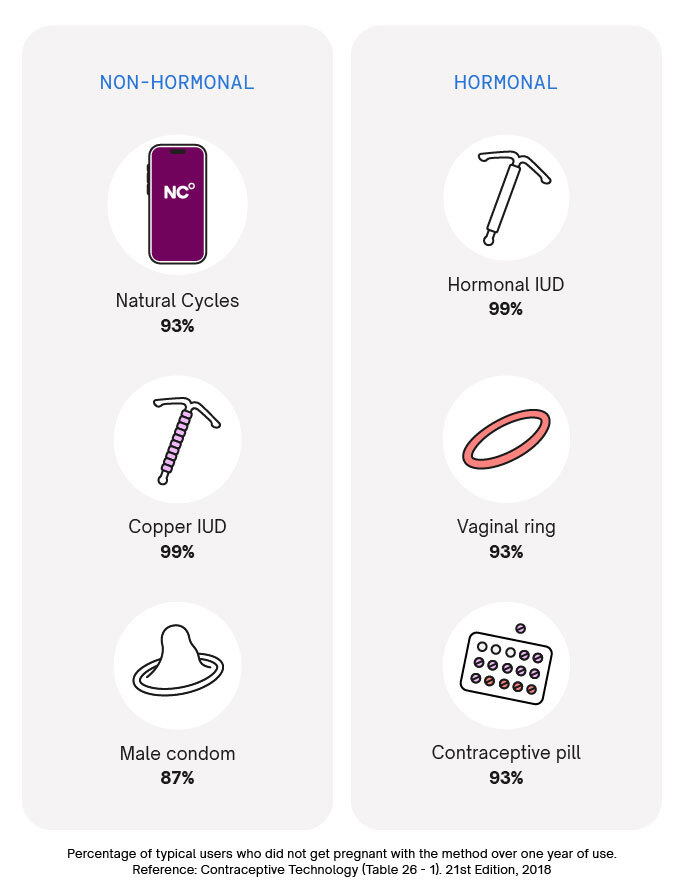
What are some effective birth control methods?
Let’s take a closer look at some effective birth control. But remember that, of course, these are just a selection of contraceptive methods, there are many more options of birth control available. The World Health Organization provides a longer list of birth control methods and the numbers around typical use and perfect use — check it out here [3].
Natural Cycles
Natural Cycles is a non-invasive, non-hormonal form of birth control. It uses basal body temperature data, period data, and optional luteinizing hormone (LH) tests to calculate your daily fertility status. Red Days are days when you may be fertile. On all Red Days, you should use barrier protection (we recommend condoms) or abstain from vaginal intercourse. Green Days are when you’re not fertile, and no additional protection is needed.
Things to know about Natural Cycles:
- Natural Cycles has a typical use effectiveness rate of 93% and perfect use effectiveness of 98%.
- In 2018, the FDA cleared Natural Cycles as the first contraceptive app, making birth control history. It remains the only FDA Cleared birth control app on the market today.
- When you start using Natural Cycles, it can take some time to get to know your unique cycle, resulting in an increased number of Red Days during your first 1-3 cycles. This ensures that the app is effective from the first day of use. Once Natural Cycles has detected your ovulation, you are likely to receive more Green Days. You can rely on the fertility status indicated by the app from the first day of use.
- Natural Cycles is still effective if you have irregular periods, although if you have a very irregular cycle (longer than 35 days), it may give you more Red Days. However, many people find it useful as a way of tracking symptoms and better understanding their bodies. [4]
Barrier Methods
Barrier methods of contraception work by physically or chemically blocking sperm from reaching the egg to prevent pregnancy.
Condoms
When you hear “condoms”, it’s likely you think of the external, male condoms – but there is also another, less common type, the internal condom. External condoms are worn on the penis during penetrative vaginal sex to prevent pregnancy. They work by acting as a barrier, stopping sperm from entering the vagina and subsequently reaching the egg released every cycle.
Things to know about condoms:
- With typical use, external or male condoms are 87% effective. That’s because people don’t always follow instructions, the condom sometimes breaks, and sometimes people forget to use condoms altogether. With perfect use, they’re 98% effective. [2]
- Many methods of birth control don’t protect against sexually transmitted infections – but condoms do. They’re over 90% effective against HIV, Hepatitis B, and gonorrhea, and also significantly lower the risk of getting several other infections like chlamydia and syphilis. [5]
- Internal condoms, also called female condoms, are worn inside the vagina and are 79% effective with typical use. [2] While these condoms are technically less effective, some people prefer these as they give the female partner more control when using barrier methods.
Diaphragms
Diagrams are another barrier method of contraception. These are a circular dome made from soft, malleable silicone that you insert into your vagina before sex. It works in essentially the same way as condoms — by acting as a barrier that prevents sperm from reaching an egg.
Things to know about diaphragms:
- They’re 83% effective with typical use, and 84% effective with perfect use. [2]
- Unlike condoms, diaphragms don’t protect against STIs, so condoms should also be used alongside this type of birth control. [6]
- A healthcare provider must fit the diaphragm initially to ensure the correct size. Periodic refitting may be necessary, especially after childbirth or significant weight changes.
- They’re suitable for most people, but may not be right for you if you can’t reach your cervix, have ever had toxic shock syndrome, or have weak vaginal muscles. [7]
Permanent birth control
Permanent birth control, also known as sterilization, refers to medical procedures that permanently prevent individuals from being able to conceive children.
Tubal ligation
Sometimes referred to as “getting your tubes tied”, tubal ligation is major surgery in which a woman's fallopian tubes are cut, tied, or sealed to prevent eggs from reaching the uterus for fertilization.
Things to know about tubal ligation:
- Tubal ligation is over 99% effective at preventing pregnancy, meaning that fewer than 1 person out of every 100 who has the procedure will get pregnant in a year. [8]
- You’ll still have a normal menstrual cycle, until you go through menopause.
- It’s a permanent procedure although there’s a small chance that it can be reversed, it doesn’t always work. [9]
Vasectomy
Male sterilization is known as a vasectomy, sometimes called “getting the snip”. During the procedure, a man's vas deferens (the tubes that carry sperm from the testicles to the urethra) are cut, tied, or sealed to prevent sperm from entering the semen.
Things to know about vasectomies:
- As with tubal ligation, vasectomies are over 99% effective at preventing pregnancies. [2]
- But they’re not immediately effective – a semen sample is tested at least 12 weeks after to check that it doesn’t contain sperm after the procedure. [10]
- As with tubal ligation, vasectomies are meant to be permanent procedures, and while it can sometimes be reversed, it can be a complicated (and expensive) procedure, and it doesn’t always work. The surgical procedure for vasectomy reversal is successful in around 85 out of 100 people – but after a vasectomy reversal, only around 55 out of 100 partners get pregnant in practice. [11]
Long-acting reversible contraception (LARC)
Long-acting reversible contraceptives are birth control methods that offer extended protection against pregnancy without the user needing to do anything — but they’re not permanent methods like sterilization.
Implant
The contraceptive implant is a small plastic rod that’s inserted under the skin of your upper arm. It releases a synthetic version of the hormone progesterone into your bloodstream to prevent pregnancy, as it works to stop ovulation and thickens the cervical mucus to prevent sperm from reaching an egg cell. [12]
Things to know about the implant:
- The implant is more than 99% effective. Typical and perfect use don’t really apply to this type of birth control, as once it’s inserted, there isn’t anything else for the user to do. [2]
- Contraceptive implants don’t contain estrogen, so it may be a preferable option for those who can’t take this hormone, such as those who are over 35 and a smoker, prone to certain types of migraine, or have poor circulation. [12]
- Fertility typically returns quickly after the implant is removed, and it’s possible to get pregnant as early as a week after removal. [12]
Intrauterine device (IUD)
There are two kinds of IUD: the hormonal IUD and copper IUD. Both are small T-shaped devices that are inserted inside the uterus, where they prevent pregnancy, but both work in a slightly different way.
Things to know about IUDs:
- Hormonal IUDs are made of plastic and release synthetic progesterone to stop ovulation and thicken cervical mucus.
- Copper IUDs are made of copper, which also thickens mucus to prevent sperm from reaching the female egg cell, and prevents implantation of a fertilized egg cell.
- Both types of IUD are more than 99% effective. [2]
- Both are long-lasting: hormonal IUDs can be left in for up to 8 years, and copper IUDs for up to 12. [13, 14]
- Copper IUDs are a form of non-hormonal birth control, so may be suitable for those who can’t or don’t want to use hormones.
Pills and other hormonal methods
The birth control pill is probably the most well-known form of birth control, but there are other hormonal options available that aren’t as long-lasting as a hormonal IUD or implant.
Birth control shot
The birth control shot is an injection that’s given in your buttocks, upper arm, thigh, or tummy. It contains a synthetic form of the hormone progesterone which prevents pregnancy.
Things to know about birth control shots:
- With typical use, the shot is around 96% effective — and it’s over 99% effective with perfect use. [2]
- Depending on the brand used, it can last for as long as 13 weeks. [15]
- You can start using it at any time in your cycle. If you get it in the first 7 days after starting your period, you’ll be protected against pregnancy immediately, but if you get it at any other time, you’ll need to use another form of birth control for a week to ensure you’re fully protected.
- It can affect your fertility for up to a year after you stop taking the shot, so it may not be the right birth control for you if you’re planning to get pregnant in the near future. [16]
Birth control pills
Birth control pills are one of the most commonly prescribed methods of birth control, but there are actually two types of pill: the combination birth control pill and the progestin-only pill. The combination birth control pill contains both estrogen and progestin, which work together to prevent ovulation, thicken cervical mucus, and thin the uterine lining, making it less likely for pregnancy to occur. The progestin-only pill, also known as the mini-pill, contains only progestin and primarily works by thickening cervical mucus and thinning the uterine lining.
Things to know about birth control pills:
- Both types of pills are 93% effective with typical use and more than 99% effective with perfect use. [2]
- There are several things that can make the pill less effective, including vomiting, taking medication that interferes with how the pill works, and skipping one or more pills. [17]
- If you start taking the combined pill during the first five days of your cycle, you’ll be protected against pregnancy immediately, but if you start taking it any later than day five of your cycle, you should use another method of contraception for seven days until you’re fully protected.
- Progestin-only pills are fully effective after taking them for two consecutive days, no matter where you are in your cycle. [18]
Vaginal ring
The vaginal ring is a small, flexible plastic ring that’s inserted into your vagina. It releases estrogen and progesterone into your bloodstream, which stops your ovaries from releasing an egg cell, preventing pregnancy.
Things to know about the vaginal ring:
- It’s 93% effective with typical use and more than 99% effective with perfect use. [2]
- You’ll typically insert a ring and then leave it in place for 21 days, after which you have a 7-day break, before inserting a new ring. [19]
- The ring is suitable for most people, but you shouldn’t use it if you’re over 35 and a smoker, think you could be pregnant, have breast cancer or take certain medications.
What method is right for me?
The methods that have the highest typical use effectiveness ratings, and the lowest Pearl Index, are those methods that don’t require much work from the user. For example, IUDs have a very high perfect use effectiveness of more than 99%, and its typical use effectiveness is the same. That is because once an IUD is fitted, it doesn’t require any work at all from the user and so it is not impacted by user errors or forgetfulness.
Other birth control options that do require daily commitment, for example, the pill or Natural Cycles, have lower typical use effectiveness than long-acting methods, because their continued and correct use depends on us. That might be more work, but we think it’s a good thing that individuals have access to a wide selection of birth control. This means we can all have more choice to find the best option for us.
When it comes down to it, the best birth control for you is a method you can reliably use and enjoy using. Whether our birth control is hormone-free, long-acting or can prevent sexually transmitted infections are all considerations that will be less or more important to each of us.
Birth control can teach you more about your body
Here at Natural Cycles, we’re committed to closing the knowledge gap when it comes to reproductive health. This means debunking myths, sharing facts, and taking part in the wider conversation about our reproductive health.
Our birth control app is the first of its kind to be cleared by the FDA, and it works by pairing the basal body temperature method with an algorithm that learns your unique cycle. The result is a birth control that’s tailored to you. With over three million registered users worldwide, Natural Cycles is hormone-free birth control that puts you in control.
Did you enjoy reading this article?